Stroke:介入治疗大血管闭塞性卒中是有效的(独立于静脉溶栓)
2016-07-24 phylis 译 MedSci原创
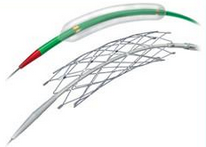
背景:在过去的十年,紧急大血管闭塞的血管内介入治疗(ELVO)发展迅速。是否静脉溶栓(IVT)预处理对ELVO患者功能预后有显著的影响仍不清楚。方法:研究对所有评估血管内治疗(ET)对急性缺血性卒中的疗效的随机对照试验,进行了系统的综述和荟萃分析。研究者按照IVT预治疗进行分层,进行的混合效应亚组分析报告,对ET(与标准治疗)与3功能结果的相关性的OR值。结果:纳入六项随机对照试验,包括1916
背景:在过去的十年,紧急大血管闭塞的血管内介入治疗(ELVO)发展迅速。静脉溶栓(IVT)预处理是否对ELVO患者功能预后有显著的影响仍不清楚。
方法:研究对所有评估血管内治疗(ET)对急性缺血性卒中的疗效的随机对照试验,进行了系统的综述和荟萃分析。研究者按照IVT预治疗进行分层,进行的混合效应亚组分析报告,对ET(与标准治疗)与3功能结果的相关性的OR值。
结果:纳入六项随机对照试验,包括1916例(49.1%接收ET 和IVT预治疗,5.6%接收ET治疗无IVT预治疗)患者。在亚组分析中,在IVT预治疗组(OR 1.83;95%CI,1.37-2.44;P<0.001)和非IVT治疗组(OR 2.47;95%CI,1.32-4.63;P = 0.001)中,ET与3个月良好功能预后相关。研究者记录IVT预治疗对行ET治疗的ELVO患者3功能预后无明显影响,提示ET对所有ELVO患者有效。IVT预处理组存在异质性(I(2)= 68.3%;Cochran Q = 0.014),未接受IVT预处理的亚组无异质性(I(2)= 0%, Cochran Q = 0.927)。对纳入试验进行定性评估发现,偏倚风险普遍较低。
结论:研究结果为临床治疗提供了依据,独立于IVT,ELVO患者接受ET治疗是有效的。
原始出处:
Tsivgoulis G, Katsanos AH, et al. Mechanical Thrombectomy Improves Functional Outcomes Independent of Pretreatment With Intravenous Thrombolysis. Stroke. 2016 Jun.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管闭塞#
46
#闭塞性卒中#
39
#静脉#
33
好文值得点赞!继续关注学习。
78
#大血管#
36