CORR:全膝置换术中自体血回输并不能降低术后输血量
2013-05-29 CORR 丁香园
骨科手术中全膝置换术是一个失血相对较多的外科手术,有文献报道全膝置换术中和术后其输血的概率分别为12%及87%,平均输血量2U。有鉴于输血过程中容易出现的不良反应较多,外科医生倾向于在术前对血红蛋白较低的患者进行术前自体血液储备或术中自体血回输。尽管目前自体血回输系统在临床应用中已经非常广泛,但其对减少术后输血的作用仍不明确,有效或无效均有文献报道,但因各个临床实验方法的不统一性,很难对目前发表的
骨科手术中全膝置换术是一个失血相对较多的外科手术,有文献报道全膝置换术中和术后其输血的概率分别为12%及87%,平均输血量2U。有鉴于输血过程中容易出现的不良反应较多,外科医生倾向于在术前对血红蛋白较低的患者进行术前自体血液储备或术中自体血回输。尽管目前自体血回输系统在临床应用中已经非常广泛,但其对减少术后输血的作用仍不明确,有效或无效均有文献报道,但因各个临床实验方法的不统一性,很难对目前发表的临床文献进行全面系统地比较。近日有澳大利亚的学者就TKA术中自体血回输是否可以减少患者术后输血量及输血概率进行了较大样本的前瞻性,随机,对照研究,相关结论发表于近期的CORR杂志上。
研究者在研究中着重解决以下问题:自体血回输洗涤红细胞(WSB)是否可以减少术后遗体血的使用;洗涤红细胞重新输入患者体内后血红蛋白值的连续变化情况;使用自体血回输系统术后是否会增加感染率。
共151例全膝置换术患者纳入研究,按随机分组原则进行试验分组:组别1,试验组,使用自体血回输系统在术前至术后6小时内进行自体血回输,共76例患者;组别2,对照组,不使用自体血回输系统,共75例患者。两组患者中分别有6例及5例患者无法获得试验数据而未纳入统计中。统计的数据包括:人口学资料,既往史(冠心病,抗凝药物使用,ASA评级),术前,术后血红蛋白水平,手术时间,术后异体血输注量,自体血输注量,早期并发症(过敏,创面感染,大或小出血,深静脉血栓,神经损伤,肺栓塞)。
所有患者术中均不使用止血带,采用内侧髌骨旁入路,所有患者均使用相同的全膝关节假体和麻醉技术,术前半小时患者接受头孢呋辛针1500mg iv作为预防用药。组别1,术中至术后6小时内进行自体血回输,组别2 无特别处理。术后第1天至第42天40mg 低分子肝素抗凝。同时在术后第1天即开始被动康复功能锻炼。
术后患者接受输血治疗的指征为:患者有贫血的临床表现,如头晕,低血压,心动过速等,同时患者血红蛋白浓度<8g/dl。监测患者术前,回输WSB后2小时,术后3天,5天时患者的血红蛋白水平。
研究结果提示:
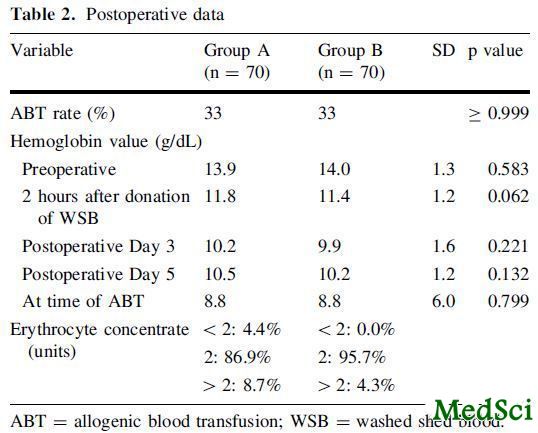
两组患者在人口统计学,手术时间,年龄,术前疾病,ASA评分等方面无显著差异,如表1所示。
两组患者在术后接受异体血输血治疗方面无显著差异(P=0.999),其中组别1,2接受异体血输血比例均为33%(23/70),平均输异体血量为2.1U,如表2所示。所有异体血输血均在术后第2-5天内完成。
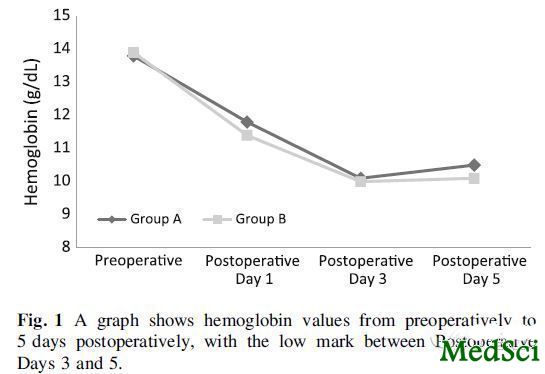
两组患者在输异体血时的血红蛋白水平无显著差异(p=0.799)。组别1平均自体输血量为283ml,其在术后2小时时的血红蛋白浓度稍高于组别2(p=0.062),但在术后3天及5天时无显著差异,如图1所示。其中组别1中发现1例自体血回输后的过敏反应。
两组患者在术后并发症方面无显著差异。
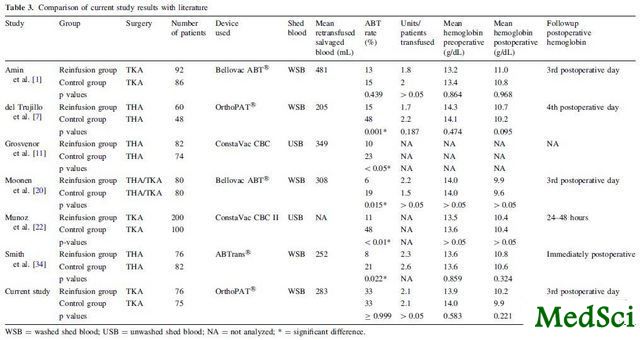
研究者在讨论中总结分析:尽管本实验存在着不足,如研究纳入的病例数较少;术中患者失血指标未纳入考察等,但鉴于试验的前瞻性,随机研究设计方案,试验结论证据强度较高,可信程度好。和以往的部分研究不同(表3),本研究统计结论发现术中进行自体血回输并不能显著降低术后的异体输血概率和输血量,研究者认为可能是真空自体血回输系统在回输过程中有额外的人体红细胞丢失,所以在临床数据上看到回输后2小时内患者的血红蛋白有升高趋势,但无明显统计学差异。
有鉴于此,研究者在最后给出了围TKA手术期血液管理的建议:对择期行TKA的患者,术前8周测量患者的血红蛋白水平,如果必要,使用静脉内补铁或EPO等方式促进血红蛋白恢复至需要值;此外,若无明显手术禁忌,可在术中单次应用凝血酸减少出血;术后6小时监测血红蛋白水平,若值>9.5g/dl,则只需要在出现贫血症状时监测血常规;若<9.5g/dl,则每天进行监测,若持续下降,血红蛋白水平<8g/DL,则行限制性输注异体血红细胞,据患者一般情况调整输注红细胞的量。
[编者按]:围手术期血液管理是一门高深的学问,至少在我这种菜鸟看来是的。其实每次麻醉科医生在鼓捣自体血回输机时我都在想,真的有效么,这是我和麻醉医生之间的争论,但至少从麻醉科医生经验角度来说应该是有效的,这个文章倒是给我和麻醉医生的争论做出了一个强力回应,同时也给我们一些提醒,有些东西看上去很美好,实际很糟糕。本文认为自体血回输不能降低术后输血概率和输血量的原因分析我还想补充一点:红细胞在非人体血管系统内的流动存在一定损伤,损伤红细胞的寿命缩短,超过红细胞正常代谢速度,可以造成血红蛋白含量的下降,这个研究的试验结果也可以说明这一点:回输后2小时内患者的血红蛋白有升高趋势,证明血液回收红细胞有一定效果;但在术后3天和5天,因血液中红细胞血红蛋白裂解破坏增多,血红蛋白水平无差异。想证实这个问题很简单,术后3天或5天测定血红蛋白的同时测点总胆红素水平。
额外补充的一点是,本文在统计测量中并没有将失血量纳入比较范围内倒是让这个结论没有像作者说的那么坚定,至于失血量未纳入统计分析对最终试验结果的影响几何倒是仁者见仁了。

Does single use of an autologous transfusion system in TKA reduce the need for allogenic blood?: a prospective randomized trial.
BACKGROUND
Mechanical autotransfusion systems for washed shed blood (WSB) were introduced to reduce the need for postoperative allogenic blood transfusions (ABTs). Although some authors have postulated decreased requirements for ABT by using autologous retransfusion devices, other trials, mostly evaluating retransfusion devices for unwashed shed blood (USB), verified a small or no benefit in reducing the need for postoperative ABT. Because of these contradictory findings it is still unclear whether autologous retransfusion systems for WSB can reduce transfusion requirements.
QUESTIONS/PURPOSES
We therefore asked whether one such autologous transfusion system for WSB can reduce the requirements for postoperative ABT.
METHODS
In a prospective, randomized, controlled study, we enrolled 151 patients undergoing TKA. In Group A (n=76 patients), the autotransfusion system was used for a total of 6 hours (intraoperatively and postoperatively) and the WSB was retransfused after processing. In Control Group B (n=75 patients), a regular drain without suction was used. We used signs of anemia and/or a hemoglobin value less than 8 g/dL as indications for transfusion. If necessary, we administered one or two units of allogenic blood.
RESULTS
Twenty-three patients (33%) in Group A, who received an average of 283 mL (range, 160-406 mL) of salvaged blood, needed a mean of 2.1 units of allogenic blood, compared with 23 patients (33%) in Control Group B who needed a mean of 2.1 units of allogenic blood.
CONCLUSIONS
We found the use of an autotransfusion system did not reduce the rate of postoperative ABTs.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#置换#
23
#输血#
33
#置换术#
23
#ORR#
21