Alzheimer Dementia : 宣武医院:双侧听觉处理障碍,或可反映认知减退
2021-10-05 Freeman MedSci原创
阿尔茨海默病(AD)患者通常抱怨在嘈杂的环境中很难跟上对话,但他们在安静的环境中却没有这个问题。这种特征性的听觉功能障碍--被称为中枢听觉处理(CAP)功能障碍--是AD的一个突出特征,它可以导致沟通
阿尔茨海默病(AD)患者通常抱怨在嘈杂的环境中很难跟上对话,但他们在安静的环境中却没有这个问题。这种特征性的听觉功能障碍--被称为中枢听觉处理(CAP)功能障碍--是AD的一个突出特征,它可以导致沟通障碍,促使社会退缩。

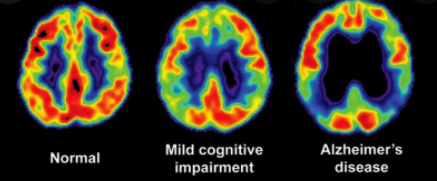
值得注意的是,多项队列研究显示,CAP功能障碍在AD发病前5到10年就已经出现。此外,CAP功能障碍还与痴呆和认知能力下降的风险增加有关。在病理学上,值得注意的是,淀粉样斑块和缠结的形成已经在听觉大脑中被检测到,即听觉神经通路的上升区域,以及大脑的初级听觉和听觉联想皮质。
多条证据支持CAP功能障碍可以被看作是AD中听觉感知和认知的一个交叉点的观点。然而,尽管取得了一些重要的研究进展,AD中CAP变化的基本方面仍然不清楚,听觉感知对认知的影响仍然难以确定。
众所周知,人类听众解析听觉场景的能力需要大脑对声音进行多层次的组织处理,包括听觉感知处理(如CAP)和认知处理(如注意、执行)。在复杂的听觉环境中,声波的混合物通过听觉知觉处理被分解成一组单独的声源,这是通过识别、分组和将复合声波隔离成独立的心理表征来实现的,每个表征被称为 "听觉对象"。
解析听觉场景的准确性取决于听觉知觉处理从声音混合物中提取听觉对象的准确性。我们知道,将复杂的信号分解成听觉对象,部分是基于计算双耳--即我们的两个耳朵各自接收的声音之间的频谱和时间关系。此外,认知处理已被证明可以根据以前的经验来组织听觉对象。一个典型的例子是 "鸡尾酒会效应",在这种情况下,听众可以不费吹灰之力地注意到一个目标语音源,在干扰的背景噪音下。值得注意的是,研究表明,对听觉信息的感知处理能力的缺陷与衰老和AD患者的语言障碍有关。
几个基本的CAP过程已经被确认,并且现在被正式认可,包括双耳处理、时间处理和听觉辨别。特别值得注意的是,双耳处理与定位声源和将声源与背景噪音分开的能力有关。双耳处理利用了声音传递到两只耳朵中的微小差异,大大提高了我们识别听觉对象和确定其位置的能力。众所周知,双耳处理依赖于脑干、颞叶和下顶叶以及其他神经解剖结构的正常运作。
这些都是参与AD的标志性脑区,所以很明显,神经退行性病变确实会影响听觉大脑,并可能损害双耳处理功能。在生理学上,以前已经表明,从背景噪音中识别声音目标是通过整合两只耳朵的频率相关的声音信息(即时间精细结构)来实现。众所周知,与频率有关的声音信息的表示是通过神经发射与声音的特定阶段同步来编码的,这依赖于神经活动的时间精度。神经同步性的丧失与频率相关信息处理中与衰老有关的衰退有关。因此,现有证据表明,双耳处理是可能在AD中受损的候选CAP功能。
噪声环境中的语言理解取决于中枢听觉功能,而这些功能在阿尔茨海默病(AD)中是脆弱的。双耳处理,利用两只耳朵的声音来最佳地处理退化的声音信息;它的特点在AD中还不太了解。
藉此,宣武医院的Changming Wang等人,对此问题进行探究。
他们在121名参与者中研究了双耳处理的行为和电生理改变(AD=27;amnestic轻度认知障碍[aMCI]=33;主观认知下降[SCD]=30;认知正常[CN]=31)。
他们观察到AD和aMCI的双耳处理能力受损,并检测到相位同步性的U型曲线变化(从CN到SCD和到aMCI下降,但从aMCI到AD上升)。

这种伴随着更严重的认知阶段的相位同步性的改善,可能反映了对双耳处理的神经适应。
此外,在明显发生神经适应的阶段,相位同步性的提高与记忆力下降有关。这些发现支持一个假设,即双耳处理缺陷的神经适应可能会加剧认知障碍,这可能有助于确定AD的生物标志物和治疗目标。
原文出处:
Wang C, Wang Z, Xie B, et al. Binaural processing deficit and cognitive impairment in Alzheimer’s disease. Alzheimer’s & Dementia. Published online September 27, 2021:alz.12464. doi:10.1002/alz.12464
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#认知减退#
49
#dementia#
32
#宣武医院#
42
学习
58
#双侧#
45