Am J Gastroenterol:胰腺病变诊断标志物: MUC5AC
2016-11-20 MedSci MedSci原创
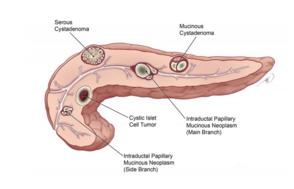
胰腺癌(PC)是一种致命的恶性肿瘤,缺乏具体的诊断标志物。本研究的目的是,调查过度表达分泌黏蛋白MUC5AC,单独或联合CA19-9的诊断力度。 通过免疫组织化学评估良性胰腺病理、PC前期病变、原发性PC组织和转移病灶中MUC5AC表达情况。使用夹心ELISA法测定循环MUC5AC水平,采用放射免疫分析法测定CA19-9。使用联合组(n=346)数据评估MUC5AC水平的诊断(n=241)和
胰腺癌(PC)是一种致命的恶性肿瘤,缺乏具体的诊断标志物。本研究的目的是,调查过度表达分泌黏蛋白MUC5AC,单独或联合CA19-9的诊断力度。
通过免疫组织化学评估良性胰腺病理、PC前期病变、原发性PC组织和转移病灶中MUC5AC表达情况。使用夹心ELISA法测定循环MUC5AC水平,采用放射免疫分析法测定CA19-9。使用联合组(n=346)数据评估MUC5AC水平的诊断(n=241)和预测(n=105,总样本201,来自手术前、后和化疗子集)效果。使用梅约诊所(n=94)和匹兹堡大学医学中心(n=321)数据,对结果进行验证。
组织表达分析表明,胰腺上皮内癌前病变1A(PanIN1A)中存在MUC5AC重新表达;进展到浸润性腺癌的所有阶段中均维持MUC5AC的表达。手术切除的早期PC(EPC)(1/2期;67.2 ng/ml, IQR: 23.9–382.1)和不能手术切除的晚期pc(LPC)(3/4期;389.7 ng/ml, IQR: 87.7–948.6)中的中位数循环MUC5AC水平均高于良性病变对照组(CP)(7.2 ng/ml, IQR: 0.4–26.5;P ≤0.0001)和慢性胰腺炎(CP)对照组(8.4 ng/ml, IQR: 1.5–19.2;P ≤0.0001)。
诊断组(n=241)数据显示,根据MUC5AC水平可有效区分EPC和健康对照组(HC)(敏感性(SN)/特异性(SP):83%/80%)以及BC(SN/SP:67%/87%)和CP(SN/SP:83%/77%)。梅约诊所和匹兹堡大学医学中心的数据验证了MUC5AC水平区分EPC和BC(68%/73%; 65%/83%)、CP(68%/79%; 65%/72%)的诊断潜力。联合MUC5AC和CA19-9可显著改善可切除病例的诊断精确度(P ≤0.0001)。
MUC5AC是一个有价值的诊断标志物,不管是单独使用还是联合CA19-9,都可以很好的区分PC和CP、良性病变。
原始出处:
Sukhwinder Kaur.et al.A Combination of MUC5AC and CA19-9 Improves the Diagnosis of Pancreatic Cancer: A Multicenter Study.Am J Gastroenterol advance online publication 15 November 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#AST#
34
#GAS#
32
#诊断标志#
38
#标志物#
34
#诊断标志物#
28
#Gastroenterol#
22