BMC Cancer:多中心倾向匹配分析比较术前 vs 术后放化疗治疗局部进展胃癌患者的疗效
2022-02-28 yd2015 MedSci原创
研究表明,局部进展期胃癌患者中术前放化疗(CRT)要优于术后CRT。
围手术期放化疗在局部进展期胃癌中起重要作用。与术后治疗相比,术前治疗是否能改善远期预后尚不清楚。近期,苏州大学团队开展了相关研究,旨在比较局部进展期胃癌患者术前放化疗(pre-CRT)和术后放化疗(post-CRT)治疗的临床预后。相关结果发表在BMC Cancer杂志上。

从2009年1月到2019年4月,来自两个中心的222例接受术前CRT和术后CRT的T3/4期和/或N阳性胃癌患者被纳入研究。倾向评分匹配(PSM)后,采用Kaplan-Meier分析和log-rank检验比较CRT前后组的局部区域控制率(LC)、远处无转移生存期(DMFS)、无病生存期(DFS)和总生存期(OS)。
共纳入222例患者,男性患者占79.3%。平均年龄为60岁(27-75岁)。T3/4期和临床N阳性率分别为89.6和84.2%。其中术前放化疗(pre-CRT)组92例,术后放化疗(post-CRT)组130例;经过倾向评分匹配(PSM)后,两组各有60例患者。
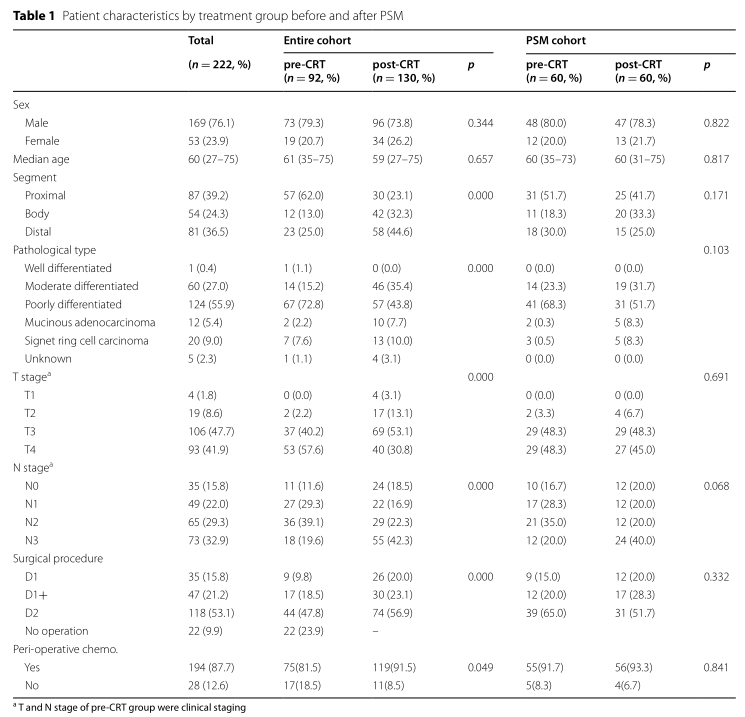
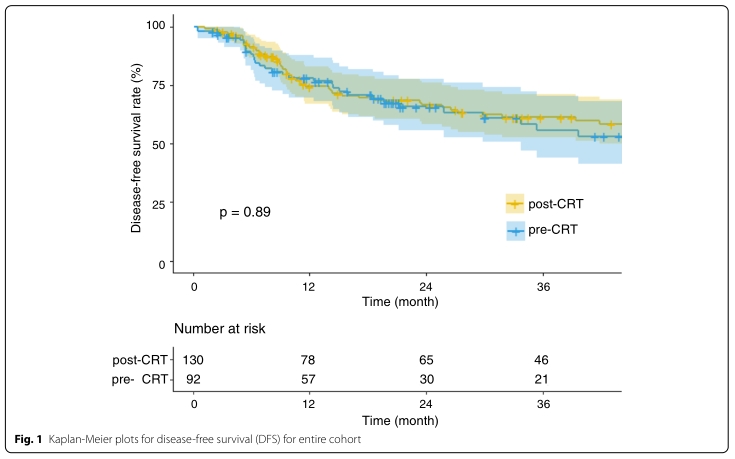
PSM前,术前放化疗(pre-CRT)组和术后放化疗(post-CRT)组的临床结果无显著差异。其中3年LC率分别为90.6%和95.6%(p=0.056),3年DMFS率分别为59.6% 和65.7%(p=0.922) ,3年DFS 率分别为56.3% 和61.2%(p=0.998),3年OS率分别为62.4%和64.5%(p=0.668)。
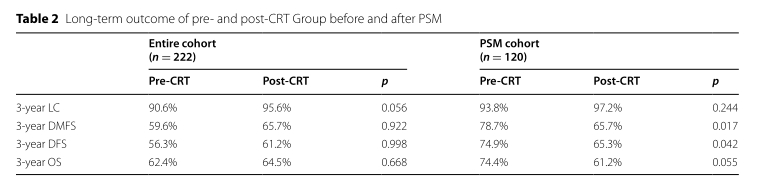
PSM后,术前放化疗(pre-CRT)组和术后放化疗(post-CRT)组患者的3年LC率分别为93.8%和97.2%(p= 0.244),3年DMFS率分别为78.7%和65.7% (p=0.017),3年DFS率分别为74.9%和65.3%(p=0.042),3年OS率分别74.4%和61.2%(p=0.055)。
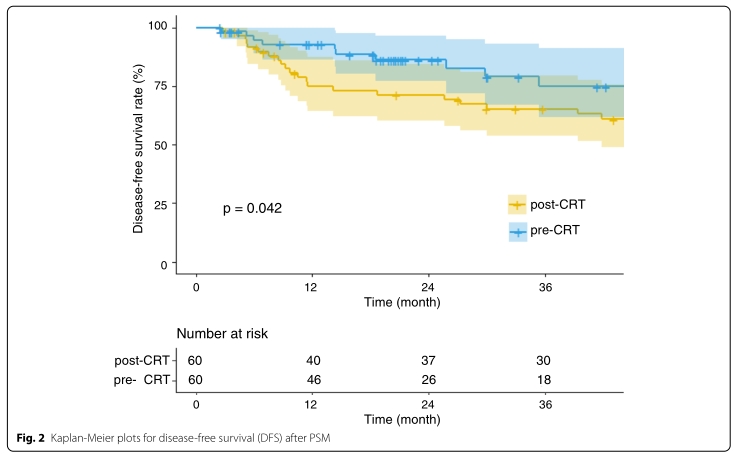
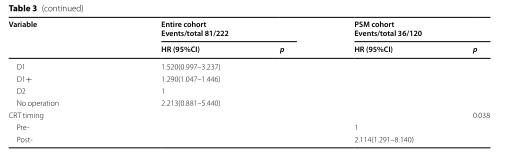
在单变量分析中,临床N期和术前CRT治疗与DFS显著相关。在PSM队列中,术前CRT治疗在多变量模型中仍具有显著性(p = 0.038)。

综上,研究表明,局部进展期胃癌患者中术前放化疗(CRT)要优于术后CRT。
原始出处:
Zhang H, Yu R, Zhang L, Wang R, Xiao L. Chemotherapy versus chemoradiotherapy for FIGO stages IB1 and IIA1 cervical squamous cancer patients with lymphovascular space invasion: a retrospective study. BMC Cancer. 2022 Feb 23;22(1):202. doi: 10.1186/s12885-022-09309-6. PMID: 35193525; PMCID: PMC8864837.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#胃癌患者#
29
#BMC#
30
#多中心#
25
#放化疗#
27
#局部#
31