病例提供者:彭毅 中国人民解放军武汉总医院
患者,男,50岁。主诉:胸痛3小时余。
现病史
患者于2017年1月23日下午17时无明显诱因下突发胸痛,位于心前区,约巴掌范围大小,为压榨感,向左侧肩部放射,伴大汗、乏力等不适。患者无发热、畏寒,无恶心、呕吐,无视物旋转、黒朦、晕厥,症状持续不缓解。
外院就诊,心电图提示“急性前壁心肌梗死”,予以拜阿司匹林 300 mg 嚼服,替格瑞洛 180 mg 口服,吗啡镇痛治疗后转入我院。病程中,患者精神、食欲、睡眠均欠佳。
既往史
体格检查
体温:36.5℃,脉搏:72次/分,呼吸:18次/分,血压:150/108 mmHg。神清,双肺呼吸音清,未闻及干湿性啰音。心界无扩大,心率:72次/分,律齐,各瓣膜听诊区未闻及杂音。腹平软,无压痛。双下肢无水肿。
辅助检查
磷酸肌酸激酶:669 u/L,肌酸激酶同工酶:52u/L,乳酸脱氢酶:203u/L,羟丁酸脱氢酶:179u/L。
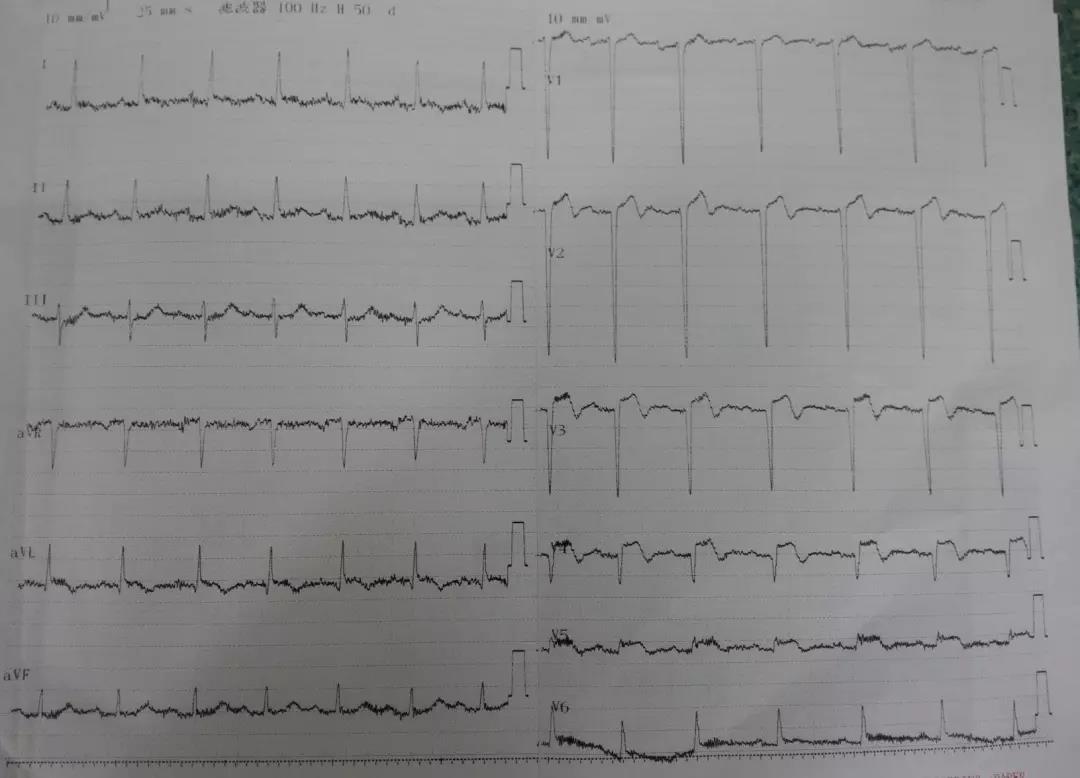
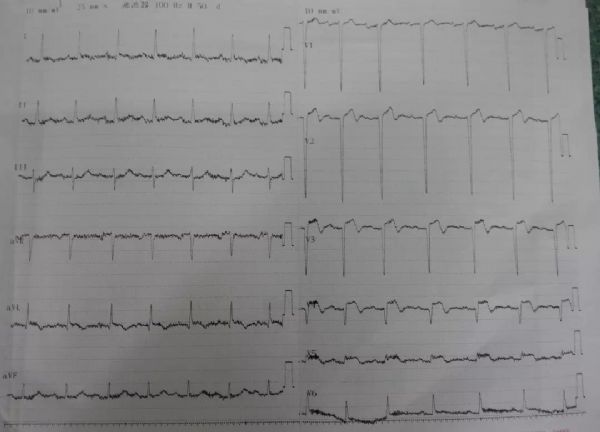
心电图:
1、冠心病,急性前壁心肌梗死,Killip I级;2、高血压病2级,极高危。
风险评分
Grace评分:67.4
Crusade评分:25,低危。
治疗经过
术前:阿司匹林 300 mg 嚼服,替格瑞洛 180 mg 口服。
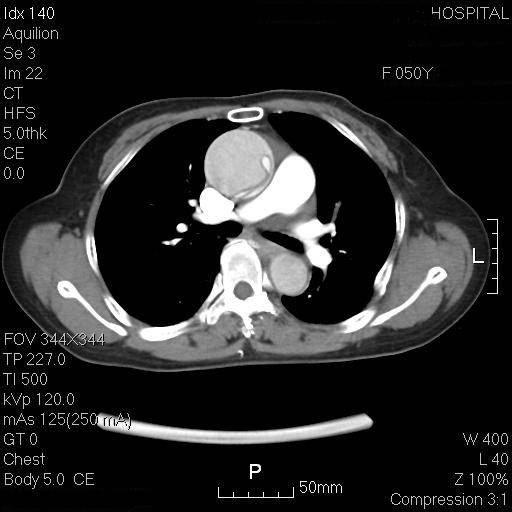
沿导引导丝插入6F EBU3.5指引导管至左冠开口,经指引导管插入SION BLUE导引导丝通过闭塞处至前降支远端。沿导引导丝将预扩球囊(Sprinter 2.5×20 mm)置于前降支中段闭塞处,以8个大气压扩张10秒,造影显示有残余狭窄,D1从该处分出,开口及近段严重狭窄约95%,退出球囊导管。
经指引导管插入SION导引导丝到D1远端,沿SION导引导丝将预扩球囊(Sprinter 2.5×20 mm)置于D1开口处及近段,以4个大气压分别扩张8秒,造影显示狭窄改善,退出球囊导管。
沿SION BLUE导引导丝插入雷帕霉素药物涂层支架(GuReater 3.5×29 mm)至前降支中段狭窄部,以8个大气压扩张14秒,造影显示原残余狭窄消失,支架贴壁良好,退出支架球囊导管及D1内SION导丝。
术中:肝素 8000 u,硝酸甘油 600 ug,替罗非班 10 ml。
主要 PCI 过程

术后用药
1、阿司匹林 100 mg qd,2、氯吡格雷 75 mg,qd,3、瑞舒伐他汀 10 mg qn,4、单硝酸异山梨酯 20 mg bid。
临床思辨
该患者既往有蛛网膜下腔出血病史,虽然出血评分不高,但并不能等同于出血风险不高。
既往有颅内出血病史,在使用双联抗血小板治疗中必须注意替格瑞洛的出血风险。PLATO研究中,替格瑞洛抗血小板治疗的出血风险高于氯吡格雷,并且在替格瑞洛的药物说明书中明确提出:既往有脑出血病史是使用替格瑞洛的禁忌症。
该患者虽然在急诊科使用了替格瑞洛抗血小板治疗,但是在PCI术后,我们仍然选用阿司匹林联合氯吡格雷双联抗血小板方案。
氯吡格雷在支架术后第1周可考虑使用150 mg/d,以减少冠脉事件发生率,1周后再改为75 mg/d。在临床实践中,我们需要根据患者的具体情况调整抗栓治疗方案,在使用抗栓药物时需要认真学习其药物说明书,防微杜渐,减少临床不良事件。
用药小贴士
新型抗血小板药物替格瑞洛,其本身为活性药物无需经肝酶代谢,可与ADP受体可逆结合,在临床上应用逐渐增加。
PLATO研究显示,替格瑞洛组和氯吡格雷组的总出血事件无显着差异,但是非CABG相关的出血事件,替格瑞洛组高于氯吡格雷组(P=0.03)。
并且,替格瑞洛组的颅内出血率高于氯吡格雷组(26例 vs 14例,P=0.06),包括致死性颅内出血(11例 vs 1例,P=0.02)。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抗血小板药#
29
#血小板药物#
46
学习谢谢分享!
73
#ACS#
53
学习了解一下
70
学习
57