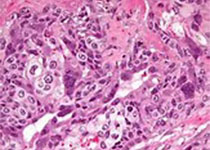
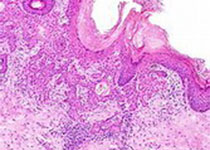
Am J Prev Med:有关乳腺癌和卵巢癌过度治疗,科学家有话说
2017-03-31 佚名 生物通
据3月22日发表在美国预防医学杂志中的文章报道,通过分析BRCA诊断这项检测10年来的各种数据,研究人员发现过多的非高风险人群参加了BRCA测试,并不利于最大化其对乳腺癌或卵巢癌的检出率,呼吁医疗界不该放松基因诊断的受试门槛。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#乳腺癌和卵巢癌#
38
#过度治疗#
51
#Med#
32
已经学习,谢谢分享!
57
签到学习了很多。
65