Nat Commun:胃肠道细菌变化可阻止中风发生
2013-05-06 ZinFingerNase 生物谷
2012年12月06日--来自瑞典查尔姆斯理工大学和哥德堡大学的研究人员证实人肠道菌群变化与表现出症状的动脉粥样硬化和中风相关联。这些研究发现于近期发表在Nature Communications期刊上。 人体含有的细菌细胞数量是人细胞的10倍多,其中大多数细菌细胞是在人肠道中发现的。除了我们的宿主基因组外,这些细菌含有大量的基因,它们一起被称作肠道宏基因组(gut metagenome)。

2012年12月06日--来自瑞典查尔姆斯理工大学和哥德堡大学的研究人员证实人肠道菌群变化与表现出症状的动脉粥样硬化和中风相关联。这些研究发现于近期发表在Nature Communications期刊上。
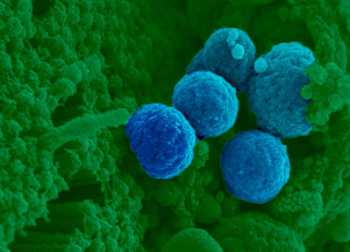
人体含有的细菌细胞数量是人细胞的10倍多,其中大多数细菌细胞是在人肠道中发现的。除了我们的宿主基因组外,这些细菌含有大量的基因,它们一起被称作肠道宏基因组(gut metagenome)。
这种宏基因组如何影响我们的健康?当前已有很多研究人员正在设法解决这个问题。在之前的研究中,科学家们已发现几种疾病与肠道宏基因组的变化相关联。如今在一项新的研究中,研究人员也证实肠道宏基因组变化与动脉粥样硬化和中风相关联。
研究人员比较了一组中风病人和一组健康人,并且发现他们的肠道菌群存在重大的差异。特别是,他们证实合成类胡萝卜素所需的基因在来自这组健康人的肠道菌群中更加频繁地发现。相对于中风存活者而言,这组健康人的血液也存在着显著性更高水平的某种类胡萝卜素。
类胡萝卜素是一类抗氧化剂,而且多年来人们一直声称它们对抗心绞痛和中风。因此,来自这组健康人的肠道细菌存在水平增加的合成类胡萝卜素的细菌可能提供线索来解释肠道宏基因组如何影响疾病状态。通过研究病人的肠道菌群,人们应当能够对心血管疾病进行风险预测。
与中风相关的拓展阅读:
- Diabetes:降糖药linagliptin可能减少中风后脑损伤
- Stroke:一种预防中风的潜在疗法
- PNAS:天然海藻化合物有望治疗中风
- Heart:减肥手术或降低患者心脏疾病和中风风险
- Neurology:食用番茄可降低卒中风险 更多信息请点击:有关中风更多资讯

Symptomatic atherosclerosis is associated with an altered gut metagenome.
Abstract
Recent findings have implicated the gut microbiota as a contributor of metabolic diseases through the modulation of host metabolism and inflammation. Atherosclerosis is associated with lipid accumulation and inflammation in the arterial wall, and bacteria have been suggested as a causative agent of this disease. Here we use shotgun sequencing of the gut metagenome to demonstrate that the genus Collinsella was enriched in patients with symptomatic atherosclerosis, defined as stenotic atherosclerotic plaques in the carotid artery leading to cerebrovascular events, whereas Roseburia and Eubacterium were enriched in healthy controls. Further characterization of the functional capacity of the metagenomes revealed that patient gut metagenomes were enriched in genes encoding peptidoglycan synthesis and depleted in phytoene dehydrogenase; patients also had reduced serum levels of β-carotene. Our findings suggest that the gut metagenome is associated with the inflammatory status of the host and patients with symptomatic atherosclerosis harbor characteristic changes in the gut metagenome.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#COMMUN#
37
#Nat#
35
#胃肠道#
37
#肠道细菌#
30