JACC:PCI时选用药物洗脱支架,可降低透析患者死亡率
2016-03-22 崔倩 译 MedSci原创
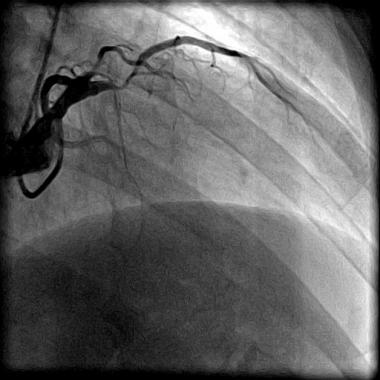
在经皮冠状动脉介入治疗(PCI)的患者中,药物洗脱支架(DES)与裸金属支架(BMS)相比可以降低再次血运重建,但其对死亡和心肌梗死(MI)的影响却是好坏参半。很少有研究侧重于终末期肾病患者进行研究。这项研究比较了在透析患者中DES和与BMS经皮冠状动脉介入治疗对于死亡率和心血管疾病发病率的影响。研究人员从USRDS(美国肾脏数据系统)确定了36117例透析患者,这些患者在2003年4月23日和2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#洗脱支架#
26
#JACC#
23
值得学习
121
#患者死亡#
28
#药物洗脱支架#
29
#ACC#
28
#透析患者#
29