梅奥经验:如何选择新型口服抗凝药?
2015-07-28 佚名 心在线微信
在7月24日的西安会上,美国梅奥医学院的Win K. Shen教授,针对新型口服抗凝药(NOAC)的药物特征,以及如何个体化用药,进行了清晰详尽的讲解。 药物特征差异 目前,美国食品与药物管理局已经批准四种NOAC上市:达比加群(IIa因子抑制剂),以及阿哌沙班、依度沙班、利伐沙班(Xa因子抑制剂)。我国批准的NOAC包括达比加群、阿哌沙班及利伐沙班。 四种药物的半衰
在7月24日的西安会上,美国梅奥医学院的Win K. Shen教授,针对新型口服抗凝药(NOAC)的药物特征,以及如何个体化用药,进行了清晰详尽的讲解。
目前,美国食品与药物管理局已经批准四种NOAC上市:达比加群(IIa因子抑制剂),以及阿哌沙班、依度沙班、利伐沙班(Xa因子抑制剂)。我国批准的NOAC包括达比加群、阿哌沙班及利伐沙班。
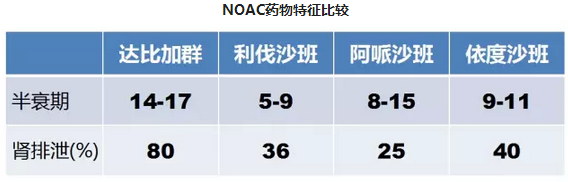
四种药物的半衰期相近,都非常短。因此,药物起效、失效快,服药频率均为qd或bid。
临床试验证据
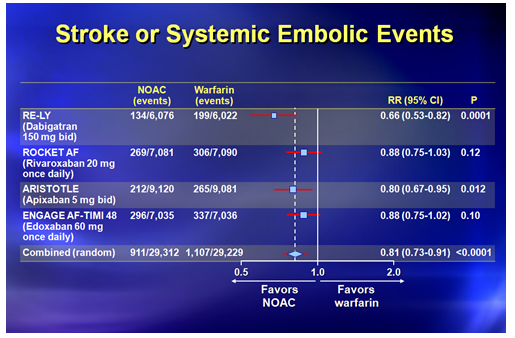
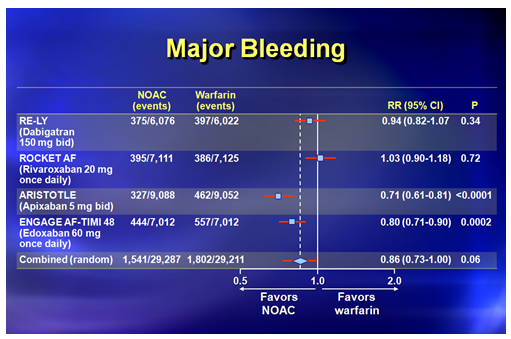
ROCKET AF研究:利伐沙班 20 mg qd vs. 华法林
RELY研究:达比加群 150 mg bid vs. 华法林
ARISTOTLE研究:阿哌沙班 5 mg bid vs. 华法林
ENGAGE AF-TIMI 48研究 依度沙班 60 mg qd vs. 华法林
对以上4项研究中超过71000例患者资料进行分析后发现:
1.脑卒中或全身性栓塞事件:NOAC不劣于华法林。
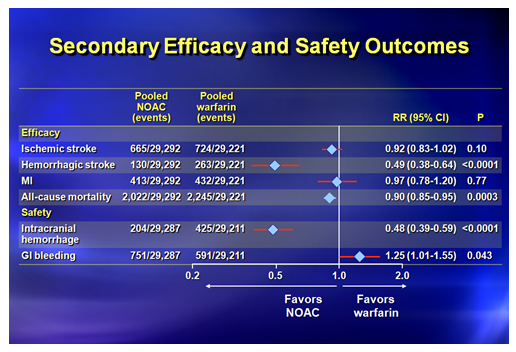
有效性
出血性脑卒中:NOAC优于华法林。
缺血性脑卒中、心肌梗死、全因死亡:NOAC不劣于华法林。
安全性
颅内出血:NOAC优于华法林。
消化道出血:NOAC劣于华法林。
1.警惕肾功能
● 4项研究均排除了肾小球滤过率(eGFR)<25-30 ml/min的患者;
● 经肾排泄率:达比加群80%,利伐沙班、阿哌沙班约30%,依度沙班约40%;
● 肾功能损伤是脑卒中、出血、死亡的独立危险因子;
● 对于>80岁的老年人,以及肾功能损伤患者(eGFR<50 ml/min),应谨慎使用达比加群150 mg bid;
● 肌酐清除率(CrCl)<50 ml/min的患者,应使用利伐沙班15 mg/d;
● 以下三项中,符合两项者,应使用阿哌沙班2.5 mg bid:年龄 80岁,体重 60 kg,肌酐 1.5 mmol/L;
● 对于eGFR>95 ml/min的患者,华法林较依度沙班更有效。
肾功能要点总结
● eGFR<50 ml/min、年龄>80岁或体重<60 kg的患者,需要调整剂量。例如,减小达比加群剂量至110 mg或75 mg bid,利伐沙班15mg qd,阿哌沙班2.5 mg bid;
● 终末期肾病(CrCl<15 ml/min或透析)患者不能使用NOAC。但是,Shen教授指出,在临床实践中,CrCl为 25-30 ml/min时,他通常就不再选用NOAC。
2.机械瓣膜不能使用NOAC
比较机械瓣膜患者使用达比加群vs. 华法林的RE-ALIGN研究发现,达比加群组的血栓栓塞事件及出血事件均高于华法林组,该试验因此提前结束。
3.抗栓治疗选择

与非亚洲人群相比,亚洲人群发生脑卒中、全身性栓塞及出血的风险更大。
如何个体化选择NOAC?
● 减少缺血性脑卒中效果最佳:达比加群;
● 经肾排泄最多:达比加群;
● 每日一次剂量:利伐沙班、依度沙班;
● 对于有轻度肾功能损伤的高危患者,有明确的剂量调整指导:利伐沙班、阿哌沙班、依度沙班;
● 严重肾功能损伤、机械瓣膜患者,应使用华法林;
● 华法林费用更低。
中国患者
● CHADS2和CHA2DS2-VASc评分未被证实;
● 随机对照试验显示,在减少脑卒中和出血风险方面,NOAC效果良好;
● 或可优先选择NOAC。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#新型口服抗凝药#
41
有人两个人问过,具体怎么用记不清,复习一下
104
#梅奥#
39
#口服抗凝药#
45
讲的不错
127