JCC:溃疡性结肠炎维持治疗期间Vedolizumab的谷浓度水平和组织学愈合相关
2019-09-02 不详 MedSci原创
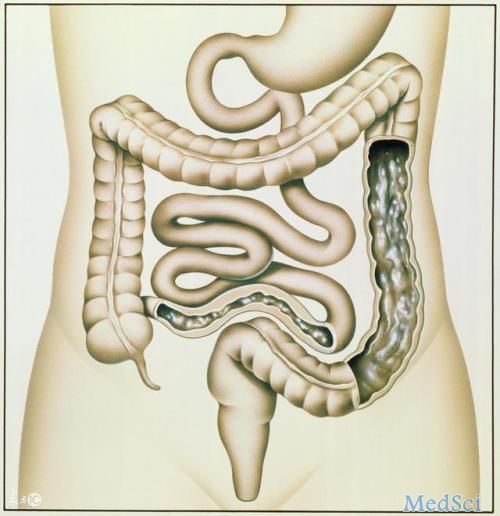
组织学愈合可能是溃疡性结肠炎[UC]的最终治疗目标。因此,研究人员就二者展开了对vedolizumab谷浓度水平与UC组织学愈合之间的关联的研究。
背景和目的
方法
本项研究是一项单中心回顾性队列研究,纳入了2014年6月至2018年间所有接受过vedolizumab维持治疗的UC患者,研究人员收集了所有的患者的临床数据,并对组织学及药物浓度进行监测。组织学愈合定义为Nancy组织学指数≤1。
结果
本项研究共分析了35个组织学样品。与没有组织学愈合的组(15 [9-26.6]μg/ mL,p = 0.02)相比,组织学愈合组(31.5 [25-49.1]μg/ mL)的维多利珠单抗水平较高。较高的vedolizumab的谷浓度与更高的组织学愈合率相关[ p = 0.10]。维多珠单抗波谷水平为截断值为25μg/ mL,其预测组织学愈合的准确度为74%,接受者操作曲线下面积为0.62 [95%置信区间0.58-0.92,p = 0.004]。双变量分析发现维多珠单抗波谷水平≥25μg/ mL [ p = 0.006],部分梅奥评分≤1[ p= 0.008,C-反应蛋白水平<5 mg / L [ p = 0.005]和Mayo内镜评分≤1[ p = 0.0004]是与组织学愈合相关的因素。
结论
在UC的维持治疗期间,组织学愈合与较高的维多珠单抗谷浓度水平相关。根据南希组织学指数参考,维多珠单抗波谷水平为25μg/ mL时被证明是预测组织学愈合的最佳选择。
原始出处:
Lieven Pouillon. Et al. Vedolizumab Trough Levels and Histological Healing During Maintenance Therapy in Ulcerative Colitis. Journal of Crohn's and Colitis.2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#溃疡性#
30
#mAb#
32
#组织学#
24
#vedolizumab#
29
#浓度#
36