Science:开发出分泌胰岛素的人工β细胞
2016-12-11 MedSci MedSci原创
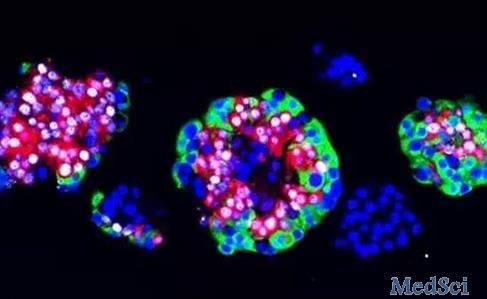
在一项新的研究中,来自瑞士苏黎世联邦理工学院和中国华东师范大学等机构的研究人员利用一种简单明了的工程学方法制造出人工β细胞。这些人工β细胞能够做天然的β细胞做的任何事情:它们测量血液中的葡萄糖浓度,产生足够的胰岛素来有效地降低血糖水平。相关研究结果发表在2016年12月9日那期Science期刊上,论文标题为“β-cell–mimetic designer cells provide closed

这些人工β细胞能够做天然的β细胞做的任何事情:它们测量血液中的葡萄糖浓度,产生足够的胰岛素来有效地降低血糖水平。相关研究结果发表在2016年12月9日那期Science期刊上,论文标题为“β-cell–mimetic designer cells provide closed-loop glycemic control”。
之前的方法都是基于干细胞开展的:科学家们通过加入生长因子或整入复杂的基因网络允许它们分化为β细胞。
对HEK细胞进行少量重编程
对研究人员的新方法而言,他们使用一种基于人肾细胞的细胞系,即HEK细胞。他们使用了HEK细胞膜中天然的葡萄糖转运蛋白和钾离子通道。他们利用一种电压依赖性钙离子通道、一种产生胰岛素或GLP-1的基因提高它们的功能,其中GLP-1是一种参与血糖水平调节的激素。
电压开关导致胰岛素产生
在这些人工β细胞中,HEK细胞的天然葡萄糖转运蛋白携带来自血液中的葡萄糖到细胞内部。当血糖水平超过某个阈值时,钾离子通道关闭。这会颠倒细胞膜上的电压分布,导致钙离子通道打开。随着钙离子流进,它触发HEK细胞内在的信号转导级联事件,导致胰岛素或GLP-1的产生和分泌。
在糖尿病模式小鼠体内对这些人工β细胞的初步测试揭示出这些细胞是非常有效的:论文共同通信作者、苏黎世联邦理工学院生物系统科学与工程系Martin Fussenegger教授说,“它们要比迄今为止世界上任何地方获得的任何方法更长时间地更好地发挥功能。”当植入到糖尿病模式小鼠体内时,这些经过修饰的HEK细胞在三周内可靠地发挥作用,产生足够数量的调节血糖水平的胰岛素或GLP-1。
有益的建模
在开发这些人工β细胞中,研究人员使用了苏黎世联邦理工学院生物系统科学与工程系教授Jörg Stelling实验室构建的一种计算机模型。这种模型允许对细胞行为进行预测,其中这些细胞行为能够通过实验加以验证。Fussenegger说,“来自这些实验的数据和利用这种模型计算出的数值几乎是相同的。”
Fussenegger和他的团队长期以来努力为糖尿病治疗提供基于生物技术的解决方案。几个月之前,他们利用来自个人脂肪组织的干细胞制造出β细胞。然而,这种技术是昂贵的,这是因为β细胞不得不为每名病人单独地制造。这种新的方法更加廉价,这是因为这种系统适合于所有的糖尿病病人。
投入市场仍有很长的路要走
不过,人们仍未确定这些人工β细胞何时会投入市场。在它们能够用于人体中之前,它们首先不得不经历多次临床试验。这种类型的临床试验是昂贵的,而且经常会持续好几年。Fussenegger估计道,“如果我们的人工β细胞清除了所有的这些障碍,那么它们可能能够在10年内投入市场。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胰岛#
29
#分泌#
24
#SCIE#
29
#β细胞#
31
nice
55
这个挺好的
0