Eur Heart J:降胆固醇疫苗为免疫对抗心血管疾病提供了新的希望
2017-06-20 枫丹白露 来宝网
在小鼠获得成功的结果之后,可能增强人体免疫抵抗高水平的胆固醇和由脂肪物质(动脉粥样硬化)积聚引起的动脉变窄的一种疫苗将可能在人身上实现应用。现在,I期临床试验已经开始看是否该发现可以转化到人类身上。
该研究今天(星期二)在欧洲心脏杂志发表,是第一个表明可以用导致身体产生抗体的分子对转基因小鼠进行免疫的方法,称为PCSK9(Proprotein covertase subtilisin / kexin型9),其在加强血液中低密度脂蛋白胆固醇(“坏”胆固醇)的清除方面发挥作用。
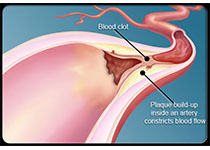
低密度脂蛋白胆固醇水平高的人,由于其遗传,或饮食不良和生活习惯差,患心血管疾病的风险过早。这些由动脉粥样硬化引起的心脏和血管疾病已经超过了感染,成为全世界疾病和死亡的主要原因。目前,他汀类药物可用于降低低密度脂蛋白胆固醇,但必须每天服用,虽然它们通常耐受性好,但可能会对某些人造成副作用。最近批准的胆固醇降低化合物是靶向PCSK9的单克隆抗体,其具有高度有效性,但其效果短暂,导致频繁的再次应用和高成本的发生。
今天发表的研究表明,在AT04A疫苗在被喂养脂肪的小鼠皮肤下注射,以诱导高胆固醇和动脉粥样硬化的发生时,使胆固醇总量降低了53%,与未接种疫苗的小鼠相比,血管动脉粥样硬化损伤减少了64%,血管炎症生物标志物降低21-28%。此外,诱导的抗体在整个研究期间保持功能,并且在研究结束时浓度仍然很高。
AFFiRis(开发AT04A的公司)首席技术官GüntherStaffler博士和研究的作者之一说:“AT04A能够在整个研究期间诱导治疗循环中针对PCSK9酶的抗体,因此,胆固醇水平以一致和持久的方式减少,导致动脉中的脂肪沉积物减少和动脉粥样硬化损伤以及动脉壁炎症减少。
“总胆固醇水平的降低与诱导的抗体浓度之间存在着显着的相关性,证明诱导的抗体导致胆固醇降低,并且最终导致动脉粥样硬化发展的减少。由于抗体浓度在研究结束时保持较高,它可以假设它们会继续减少一段时间后的胆固醇水平,导致持久的效果,正如以前的研究所示。
“如果这些发现成功地转化到人类的身上,这可能意味着,由于诱导的抗体在接种疫苗后几个月持续,我们可以开发一种持久的治疗方法,在首次接种疫苗后,只需要一年一次的加强剂,这将导致对患者有效和更方便的治疗,以及更高的患者依从性。
酶PCSK9在肝脏中产生,并锁定在LDL胆固醇受体上,降低了从血液中除去低密度脂蛋白胆固醇的能力。当注射时,AT04A导致身体产生阻断PCSK9功能的抗体,使得LDL胆固醇受体的活性增加。
“管理AT04A的方法与疫苗相当,”Staffler博士解释说。 “然而,常规疫苗与我们的方法之间的区别在于疫苗会诱导针对身体外源性的细菌或病毒蛋白质特异性的抗体 - 病原体 - 而AT04A可诱导针对由身体产生的靶蛋白的抗体 - 这是一种免疫治疗方法,而不是一种疫苗方法。“
2015年,第一期临床研究从奥地利维也纳医科大学临床药理学系开始,在72名健康人中研究AT04A和另一种分子AT06A,以评估其安全性和活性。该研究预计在今年年底完成。
德国萨尔兰大学的Ulrich Laufs教授和英国布里斯托大学的布赖恩大学教授以及美国底特律韦恩州立大学医学院的随笔社论都写道:“看来有希望进一步评估通过接种PCSK9来预防动脉粥样硬化事件,实现长期降低低密度脂蛋白胆固醇。然而,他们说“安全,人类的反应和非常重要但未知的长期免疫效应需要在临床开发过程中得到非常仔细的解决”。特别是通过他汀类药物和其他药物的总胆固醇降低与新发糖尿病的增加有关。 “因此,使用针对PCSK9的疫苗长期降低LDL胆固醇的一个潜在安全性问题是新发糖尿病风险增加的可能性。在短期内,他汀类药物和PCS9抑制剂的低密度脂蛋白胆固醇降低作用似乎是远远超过新发糖尿病的风险的。”
原始出处:
Christine Landlinger, Marianne G. Pouwer, et al. The AT04A vaccine against proprotein convertase subtilisin/kexin type 9 reduces total cholesterol, vascular inflammation, and atherosclerosis in APOE*3Leiden.CETP mice. Eur Heart J ehx260. DOI: https://doi.org/10.1093/eurheartj/ehx260 Published: 19 June 2017
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







开辟崭新的治疗思路。
35
#ART#
17
#血管疾病#
25
#HEART#
18
期待新成果造福人类。
37
学习,谢谢分享
39
学习
45