颞岛叶、鞍旁巨大生殖细胞瘤一例
2019-07-03 王莹莹 张焱 程敬亮 临床放射学杂志
患者男,35岁。因无明显诱因出现间断性头痛,枕部及双侧颞部钝痛,每次持续约20min后自行缓解,入院。MRI:右侧颞岛叶及鞍旁可见一团块状混杂短T1(图1)、稍长T2信号(图2),液体衰减反转恢复(FLAIR)序列上呈混杂稍高信号,扩散加权成像(DWI)高b值部分扩散受限呈高信号(图3),病变内可见多个大小不等的囊变区呈长T2信号,病变周围可见水肿带(图4)。静脉注入钆喷酸葡胺(Gd-DTPA)后
患者男,35岁。因无明显诱因出现间断性头痛,枕部及双侧颞部钝痛,每次持续约20min后自行缓解,入院。MRI:右侧颞岛叶及鞍旁可见一团块状混杂短T1(图1)、稍长T2信号(图2),液体衰减反转恢复(FLAIR)序列上呈混杂稍高信号,扩散加权成像(DWI)高b值部分扩散受限呈高信号(图3),病变内可见多个大小不等的囊变区呈长T2信号,病变周围可见水肿带(图4)。静脉注入钆喷酸葡胺(Gd-DTPA)后,病变呈中度不均匀强化(图5),病变累及右侧海绵窦(图6),包绕颈内动脉远端及大脑中动脉水平段近段,根据MRI考虑室管膜瘤。
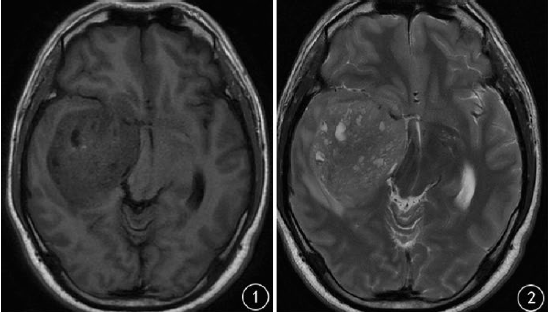
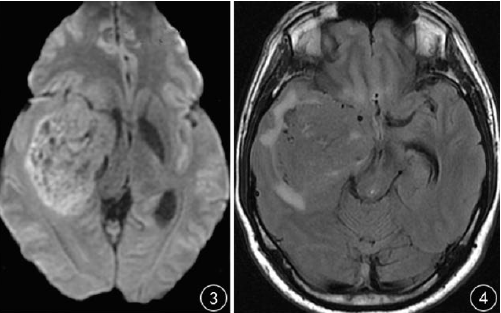
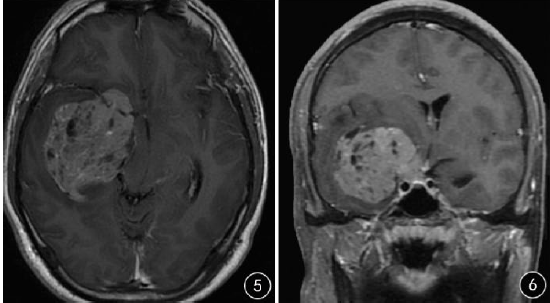
图1 轴位T1WI可见颞岛叶、鞍旁巨大肿块,内可见片状短T1信号;图2 T2WI可见病变信号不均匀,内见多个囊状长T2信号;图3 DWI高b值病变部分扩散受限呈高信号;图4 FLAIR可见病变周围轻度水肿信号;图5 增强扫描轴位,可见病变呈明显不均匀强化;图6 增强扫描冠状位,可见病变累及右侧海绵窦
术中所见:肿瘤位于右侧颞岛叶及鞍旁,灰红色,质软,血供中等,与周围脑组织无明显边界,后方与脑室脉络丛关系密切,肿瘤前内侧包绕颈内动脉。免疫组织化学染色:P53(+)、Ki-67(80%+)、CD117(+)、OCT-4(+)、SALL4(+)、PLAP(+)、Syn(-)、MPO(-),术后病理结果:生殖细胞瘤(图7)。

图7 病理图片(HE×100)
讨论
颅内生殖细胞瘤是一种少见的肿瘤,多发生于松果体区及鞍上区,或其他近中线结构,较少发生于大脑半球,颅内不同部位的生殖细胞瘤的组织病理结构基本一致,可以发生于任何年龄,但主要发生于儿童和青少年,临床症状与发生部位有关。根据其MRI表现,颅内生殖细胞瘤分为三级,Ⅰ级表现为边界不清的不伴有囊变的斑片状病变,直径<3 cm,Ⅱ级表现为伴有囊变的实性肿块,直径<3 cm,Ⅲ级表现为伴有囊变的较大实性肿块,直径>3 cm,Lee等研究发现随着肿瘤的生长,肿瘤的级别越高恶性程度越高,肿瘤内越易发生囊变、出血,肿瘤周围可无水肿或轻度水肿,占位效应较轻。
Li等研究发现磁共振波谱(MRS)对颅内生殖细胞瘤的诊断具有较大的价值,认为NAA峰、Cho峰明显增高及出现较高的Lip峰是其特征性改变。本例患者术前未行MRS检查,本例MRI表现为Ⅲ级,多发小的长T2信号是肿瘤内囊变区,肿瘤内短T1信号代表出血区,肿瘤周围轻度水肿。发生于颞岛叶、鞍旁的生殖细胞瘤需要与室管膜瘤鉴别。室管膜瘤多发生于中老年人,肿瘤多位于侧脑室旁脑实质内,瘤体边界清楚、边缘分叶,肿瘤实质部分DWI受限明显呈高信号,增强扫描肿瘤外缘大多呈显著环形强化,轻度瘤周水肿,本例MRI信号特点与室管膜瘤信号类似,但是本例患者病变呈明显不均匀强化,肿瘤外缘不呈环形强化可帮助鉴别。
总之,发生于大脑半球的生殖细胞瘤较少见,诊断较难,但MRS扫描NAA峰、Cho峰及Lip峰升高是其特征性改变,可以帮助诊断及鉴别诊断,但其最终确诊仍需病理学检查。
原始出处:
王莹莹,张焱,程敬亮,靳雅楠,汤文瑞.颞岛叶、鞍旁巨大生殖细胞瘤一例[J].临床放射学杂志,2018(03):543-544.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#生殖细胞#
39
#细胞瘤#
35
#生殖细胞瘤#
55