ASCO 2014:EGFR阳性NSCLC厄洛替尼辅助治疗DFS无获益(RADIANT研究)
2014-05-31 MedSci MedSci原创
厄洛替尼对比安慰剂用于完全切除的ⅠB-ⅢA期EGFR阳性(IHC/FISH)NSCLC辅助治疗±辅助化疗的随机双盲3期研究:RADIANT结果(A randomized, double-blind phase 3 trial of adjuvant erlotinib (E) versus placebo (P) following complete tumor resection with or
厄洛替尼对比安慰剂用于完全切除的ⅠB-ⅢA期EGFR阳性(IHC/FISH)NSCLC辅助治疗±辅助化疗的随机双盲3期研究:RADIANT结果(A randomized, double-blind phase 3 trial of adjuvant erlotinib (E) versus placebo (P) following complete tumor resection with or without adjuvant chemotherapy in patients (pts) with stage ⅠB-ⅢA EGFR positive (IHC/FISH) non-small cell lung cancer (NSCLC): RADIANT results.)
摘要号:# 7501
报告时间:2014年6月2日 9:45 AM-12:45 PM CDT(美国中部夏令时间)
Session Type:Oral Abstract Session
背景: 厄洛替尼(E)在晚期NSCLC患者中的疗效已明确,作为辅助治疗的价值有待评估。BR21研究显示EGFR阳性(IHC/FISH确诊的)的患者更能从E治疗中获益。
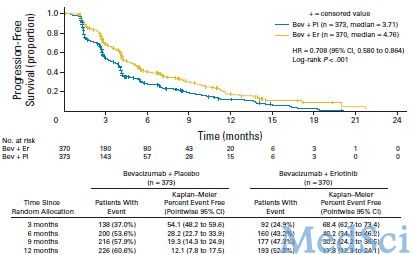
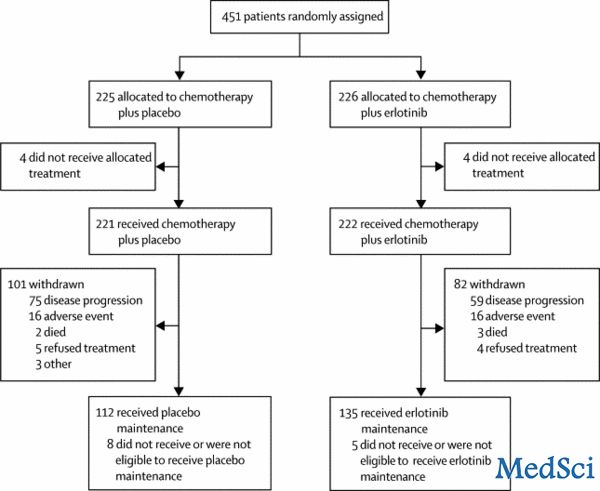
方法: 完全切除的ⅠB-ⅢA期NSCLC2:1随机入E(150mg,qd,连用2年)组和P(安慰剂)组。根据年龄,病理类型,之前是否行辅助化疗,吸烟史,EGFR状态和种族进行分层。主要研究终点为全分析集人群(FAS)的无病生存(DFS)。次要目的包括FAS的OS,以及含有del19/L858R突变(EGFR M+)类型的EGFR阳性患者的OS和PFS。
结果: 2007年11月至2010年7月,共随机入组973例患者。两组基线特征相似,年龄>6岁者占41%;女性41%;ⅠB期占51%,Ⅱ期33%,ⅢA期16% (AJCC第6版); 腺癌占59%;之前接受过辅助化疗者占53%;不吸烟者 20%;亚裔17%;EGFR FISH+ 72%,EGFR M+占16.5%。至2013年4月已达到进行最终DFS分析的计划有效事件数(410)。277(28%)患者死亡。中位随访时间47个月。
FAS分析,两组的DFS未达到统计学差异,分层分析中各次要研究终点也均未达到显著差异。E组中位治疗时间为12个月,P组为22个月。E组皮疹和腹泻的发生率分别为58%和52%,P组分别为17%和16%。≥3级的皮疹和腹泻发生率分别为:E组12.6%和6.2%,P组0.3%和0.3%。无药物相关的死亡事件。
结论: 厄洛替尼辅助治疗并不能延长总体患者的DFS,在EGFR M+患者中的疗效有待进一步证实。厄洛替尼在辅助治疗中的安全性与在晚期患者中观察到的一致。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EGFR阳性#
26
#ASC#
33
#DIA#
36
#阳性NSCLC#
28
#厄洛替尼#
26
#GFR#
23
这种术后的治疗,还应该选择传统的辅助化疗,杀伤残余肿瘤细胞,似乎更是王道。而厄洛替尼这类“抑癌”靶向药物似乎并不靠谱。虽然这些肿瘤细胞具有EGFR突变阳性,但是残余的肿瘤细胞增殖并不依赖血管新生(可以直接从周围组织中获氧),而靶向药物并不能杀死这些细胞,因此,不能推迟DFS是可以想象的,类似其它靶向药物,也应该是阴性结果。吴一龙教授似乎正在做一个类似研究。
93