JAMA Surgery:病灶大小或为无功能性胰腺神经内分泌瘤淋巴结累及的预测因子
2013-09-06 beijia688 dxy
研究要点: 放射学淋巴结状况及肿瘤分级是淋巴结转移的独立相关因素。在没有累积淋巴结情况的放射学影像证据时,NF-PanNET-G1患者的pN+风险非常低。术前肿瘤分级评估不达标时,病灶体积大小成为pN+的有力预测因子之一。 无功能性胰腺神经内分泌肿瘤(NF-PanNETs)诊断时往往表现为无淋巴结(LN)转移的无痛性肿块。因此对于低LN转移风险的患者人群,淋巴结切除术及手术范围应予限制并根据极
研究要点:
放射学淋巴结状况及肿瘤分级是淋巴结转移的独立相关因素。
在没有累积淋巴结情况的放射学影像证据时,NF-PanNET-G1患者的pN+风险非常低。
术前肿瘤分级评估不达标时,病灶体积大小成为pN+的有力预测因子之一。
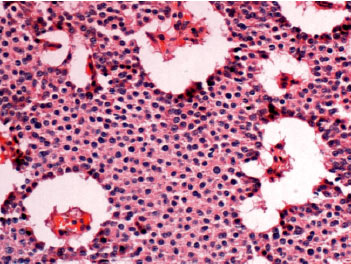
无功能性胰腺神经内分泌肿瘤(NF-PanNETs)诊断时往往表现为无淋巴结(LN)转移的无痛性肿块。因此对于低LN转移风险的患者人群,淋巴结切除术及手术范围应予限制并根据极低的复发率调整随访策略。意大利维罗纳大学Stefano Partelli博士等人对此进行了深入研究,他们证实,当不存在淋巴结累及的放射学影像特征时,NF-PanNET-G1患者的pN+风险非常低。当术前肿瘤分级评估不达标时,病灶体积大小成为pN+的有力预测因子之一。
该研究旨在建立NF-PanNETs切除术前pN+风险预测模型。在术前可用数据的基础上利用多重逻辑回归分析方法建立pN+预测模型的回顾性调查。研究检索了意大利维罗纳大学外科综合前瞻性数据库和法国Beaujon医院的临床和病理学数据。
纳入研究的受试者为1993年1月1日至2009年12月31日接受手术(R0或R1)、病理学确诊的NF-PanNETs患者。主要结局和测量指标为胰腺神经内分泌肿瘤患者的淋巴结转移风险。
结果显示,在181例患者中,有55例患者(30%)发现淋巴结转移,且与5年无病生存率下降相关。多变量分析显示,放射学淋巴结状况(rN)及肿瘤分级是淋巴结转移的独立相关因素。排除肿瘤分级后,rN及肿块直径大于4cm是淋巴结转移的独立预测因子。
研究证实,在没有累及淋巴结的放射学影像特征时,NF-PanNET-G1患者的pN+风险非常低。当术前肿瘤分级评估不达标时,病灶体积大小可成为pN+的有力预测因子之一。
研究背景:
无功能性胰腺神经内分泌肿瘤(NF-PanNETs)是一种大范围浸润的罕见肿瘤。对于此类肿瘤应利用多学科手段综合考虑患者特征和肿瘤自然史。临床上,局限于胰腺时,其一线治疗方案为手术切除,然而手术范围需要考虑风险获益的平衡而予以调整。NFPanNETs的手术路径包括标准或典型切除(如胰十二指肠切除术[PD],胰体尾切除术[DP]或全胰切除术)及非典型或保守性手术(如中段胰腺切除术(MP)或剜除术)。
中段胰腺切除术(MP)大大减少了长期胰机能不全的风险,然而术后并发症的风险也会明显升高。此外,当手术局限于单个病灶时,局部淋巴结切除术并非常规手段。LN转移对NF-PanNETs患者生存的影响尚不明确,两项TNM分类系统将pN+状态视为预后因子。
仅有40%的NFPanNETs患者诊断时出现LN转移,提示大多数患者可避免淋巴结切除术。虽然核成像技术出现了较大进展,但精确的淋巴结状态术前分类系统仍然面临挑战。pN+肿瘤风险相关术前变量的甄别对于选择最适手术方式有重要意义。本研究旨在利用成像信息为NFPanNETs建立术前pN+风险评估预测模型。
原文阅读
Partelli S, Gaujoux S, Boninsegna L, Cherif R, Crippa S, Couvelard A, Scarpa A, Ruszniewski P, Sauvanet A, Falconi M.Pattern and Clinical Predictors of Lymph Node Involvement in Nonfunctioning Pancreatic Neuroendocrine Tumors (NF-PanNETs).JAMA Surg. 2013 Aug 28
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胰腺神经内分泌瘤#
41
#神经内分泌#
30
#无功能性#
25
#分泌#
25
#功能性#
22
#GER#
36
#surgery#
28
#淋巴结#
31
#预测因子#
26
#神经内分泌瘤#
35