Am J Gastroenterol:早期穿刺术可改善新发肝硬化腹水住院患者再入院
2016-01-25 徐媛 MedSci原创
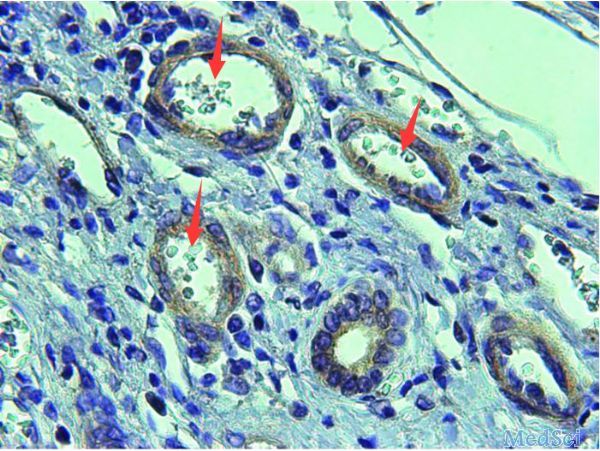
肝硬化腹水的诊断与发病率,死亡率,和减少健康相关的生活质量具有相关性,通过质量指标(QIs)可以降低患者再入院率和死亡率。研究人员通过质量指标来评估对因腹水住院的患者的治疗质量。 研究人员收纳了302名新发肝硬化腹水住院患者,并记录了入院治疗的相关临床数据,分析了患者腹水诊断30天再紧急入院的入院率和90天死亡率。 研究发现,大部分患者为男性(68.9%),年龄均超过50岁(年龄57±12.8
肝硬化腹水的诊断与发病率,死亡率,和减少健康相关的生活质量具有相关性,通过质量指标(QIs)可以降低患者再入院率和死亡率。研究人员通过质量指标来评估对因腹水住院的患者的治疗质量。
研究人员收纳了302名新发肝硬化腹水住院患者,并记录了入院治疗的相关临床数据,分析了患者腹水诊断30天再紧急入院的入院率和90天死亡率。
研究发现,大部分患者为男性(68.9%),年龄均超过50岁(年龄57±12.83 岁),其中有59%为酒精性肝硬化患者。29%的患者在30天内再次入院。30天紧急再入院率的相对风险在确诊30天内(RR 0.41,P=0.004)或住院期间(RR 0.57,P=0.006)接受腹部穿刺的患者中显著较低。90天的死亡率的独立预测因子包括年龄(OR 1.03,P = 0.03),增加了终末期肝病模型(MELD)-Na分数(OR 1.06,P = 1.06),主要SBP预防(QI7,OR 2.30,P = 2.30)和30天再入院(OR 30.26,P < 0.001)。利尿剂处方的应用会降低90天死亡率(OR 0.28,P=0.01)。71%的患者因复发性腹水在90天内再入院。总体死亡率为46%,30天再入院率是90天死亡率的一个重要预测因素。
研究结论,早期穿刺术对新发肝硬化腹水住院患者可降低30天内再入院,早期开始利尿剂治疗降低了90天的死亡率。
原始出处
Le S1,2, Spelman T3, Chong CP4, Ha P2, Sahhar L2, Lim J2, He T2, Heerasing N4, Sievert W1,2.Could Adherence to Quality of Care Indicators for Hospitalized Patients With Cirrhosis-Related Ascites Improve Clinical Outcomes?Am J Gastroenterol. 2016 Jan;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#AST#
21
#Gastroenterol#
0
#GAS#
23
#穿刺#
33
#肝硬化腹水#
26
良好的对症治疗
90
可以学习一下
80