Am J Med:冠脉造影术后急性心肌损伤高达13.5%
2016-01-17 Seven L 译 MedSci原创
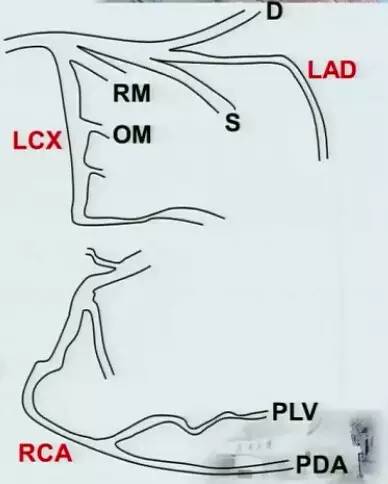
冠状动脉造影术对于冠状疾病的评估是安全的,现今全球范围内每年约有1200万名人进行冠状动脉造影术。研究者进行了一项研究,调查选择性冠状动脉造影的患者期心肌细胞损伤的频率和预测因素。该研究纳入了749名进行选择性冠状动脉造影的患者,研究者根据造影前后高敏心肌肌钙蛋白T (hs-cTnT)浓度的变化评估患者有无心肌细胞损伤,将 hs-cTnT值增高7 ng/L(满足相对变化>20%)以上定义为急性心肌
原始出处:
Kreutzinger P, Wildi K,et al.Incidence and predictors of cardiomyocyte injury in elective coronary angiography.Am J Med. 2016 Jan 4. pii: S0002-9343(15)30044-9.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#造影术#
23
学知识
86
#心肌损伤#
37
#损伤#
22
#冠脉造影#
28
#造影#
21
#Med#
15
#急性心肌损伤#
32