J Clin Oncol:PACIFIC研究5年生存结果提示放化疗后durvalumab(德瓦鲁单抗)持续改善III期NSCLC患者的预后,5年OS超过40%
2022-02-03 yd2015 MedSci原创
PACIFIC研究5年生存结果提示放化疗后durvalumab(德瓦鲁单抗)持续改善III期NSCLC患者的预后。
III期临床研究PACIFIC初步分析表明,不可切除III期非小细胞肺癌(NSCLC)患者同步放化疗后未进展患者使用durvalumab(德瓦鲁单抗)治疗可改善患者的OS (HR=0.68; 95%CI,0.53-0.87;P=0.00251)和PFS (HR=0.52; 95% CI, 0.42-0.65; P<0.0001)。近期,Journal of Clinical Oncology杂志上更新其5年生存结果。
713例随机分配的患者中,共有709例接受了durvalumab (476例中有473例)或安慰剂(237例中有236例)治疗。更新结果显示,durvalumab组的中位OS为47.5个月,安慰剂组为29.1个月(HR, 0.72; 95% CI, 0.59 to 0.89);Durvalumab组的5年OS率为42.9%,安慰剂组为33.4%。
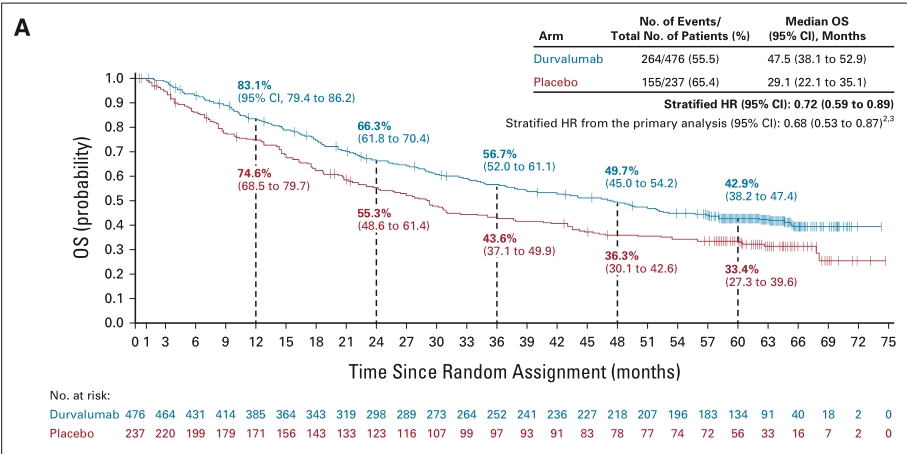
Durvalumab组的中位PFS为16.9个月,安慰剂组为5.6个月 (HR, 0.55; 95% CI, 0.45 to 0.68)。Durvalumab组的5年PFS率为33.1%,而安慰剂组为19.0%。
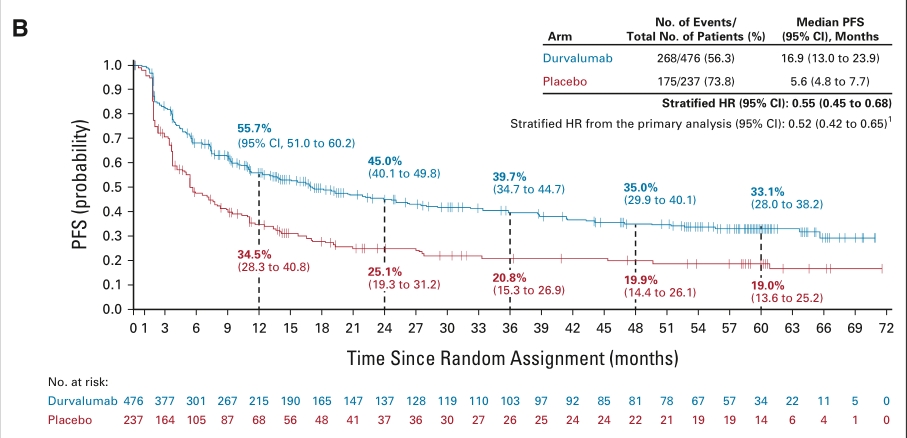
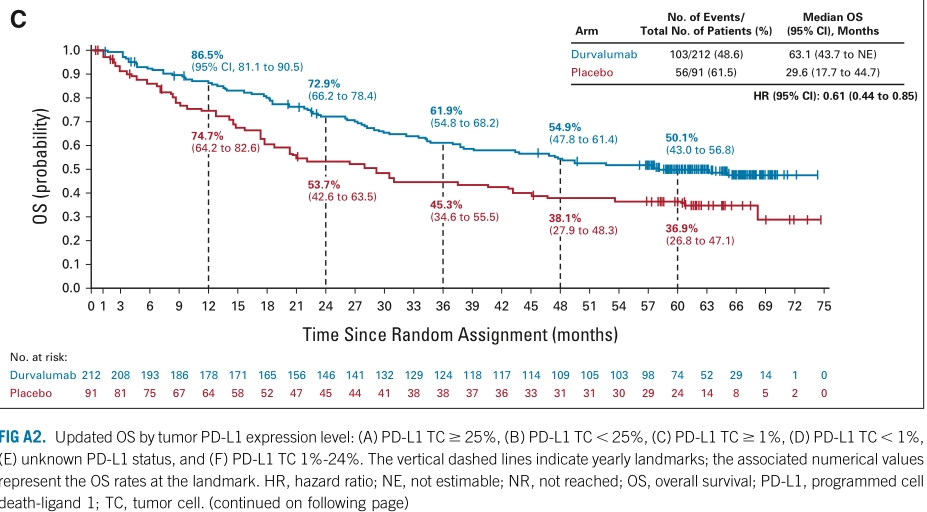
PD-L1 TC≧25%患者中, durvalumab和安慰剂组的中位OS分别为NR (43.7 to NE)和21.1 (12.6 to 46.5)个月(HR (95% CI): 0.52(0.32 to 0.82); PD-L1 TC<25%患者中, durvalumab和安慰剂组的中位OS分别为42.7 (33.1 to 52.9)和42.7 (33.1 to 52.9)个月(HR (95% CI): 0.90 (0.67 to 1.23)); PD-L1 TC≧1%患者中, durvalumab和安慰剂组的中位OS分别为63.1 (43.7 to NE)和29.6 (17.7 to 44.7)个月(HR (95% CI): 0.61 (0.44 to 0.85));
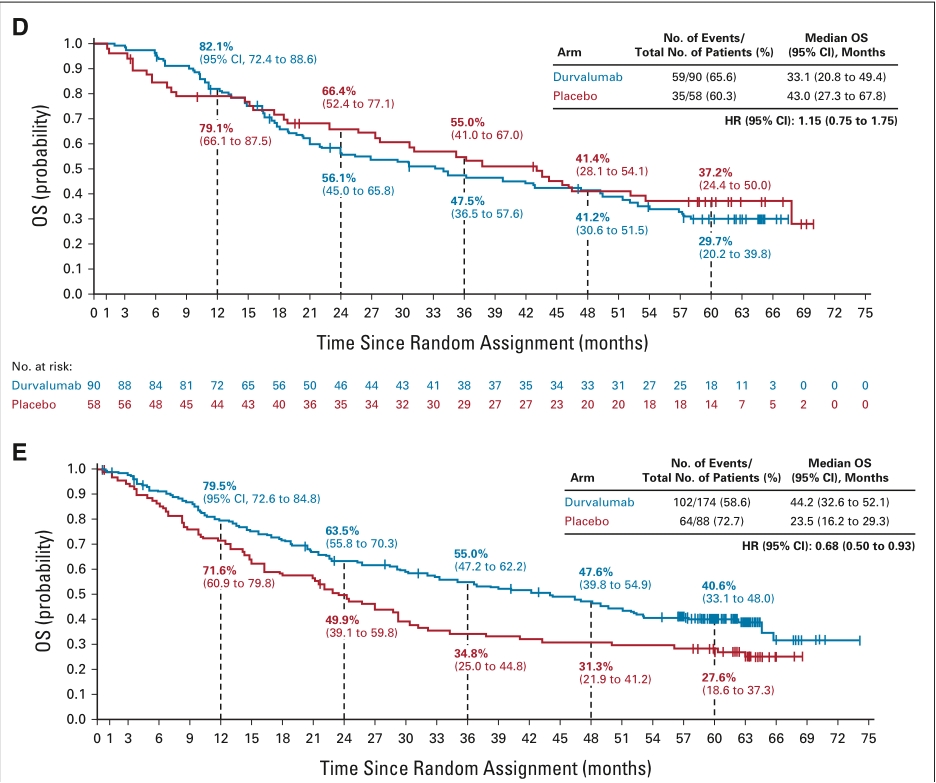
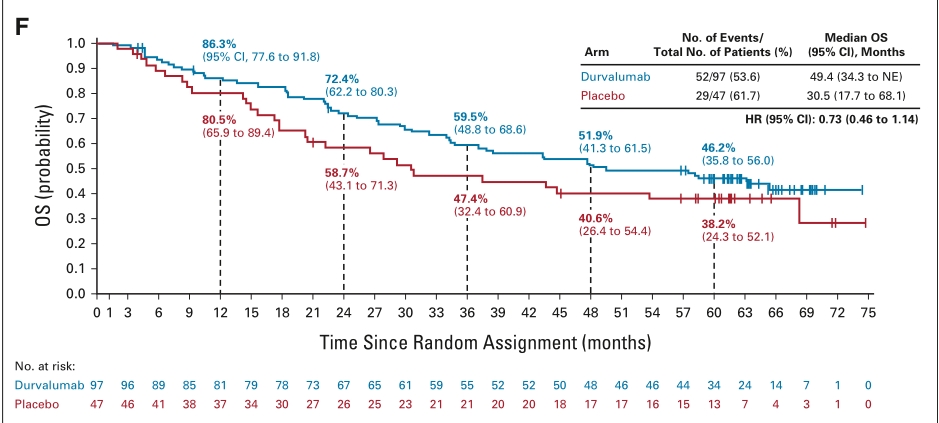
PD-L1 TC<1%患者中, durvalumab和安慰剂组的中位OS分别为33.1 (20.8 to 49.4)和43.0 (27.3 to 67.8)个月(HR (95% CI): 1.15 (0.75 to 1.75)); PD-L1不明患者中, durvalumab和安慰剂组的中位OS分别为44.2 (32.6 to 52.1)和23.5 (16.2 to 29.3)个月(HR (95% CI): 0.68 (0.50 to 0.93)); PD-L1 TC 1%-24%患者中, durvalumab和安慰剂组的中位OS分别为49.4 (34.3 to NE)和30.5 (17.7 to 68.1)(HR (95% CI): 0.73 (0.46 to 1.14))。
PD-L1 TC≧25%患者中, durvalumab和安慰剂组的中位PFS分别为25.2 (11.3 to 52.6)和3.7 (2.0 to 13.2)个月(HR (95% CI): 0.44 (0.29 to 0.67)); PD-L1 TC<25%患者中, durvalumab和安慰剂组的中位PFS分别为17.2 (11.0 to 24.9)和6.9 (5.4 to 11.0)个月(HR (95% CI): 0.64 (0.48 to 0.86)); PD-L1 TC≧1%患者中, durvalumab和安慰剂组的中位PFS分别为24.9 (16.9 to 38.7)和5.5 (3.6 to 10.3)个月(HR (95% CI): 0.47 (0.35 to 0.64));
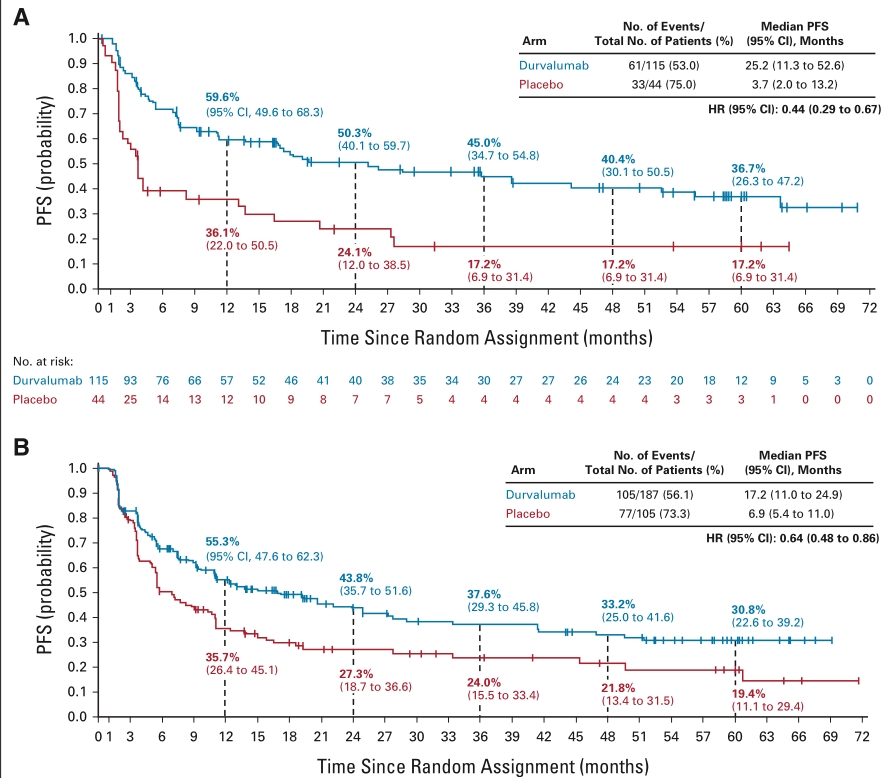
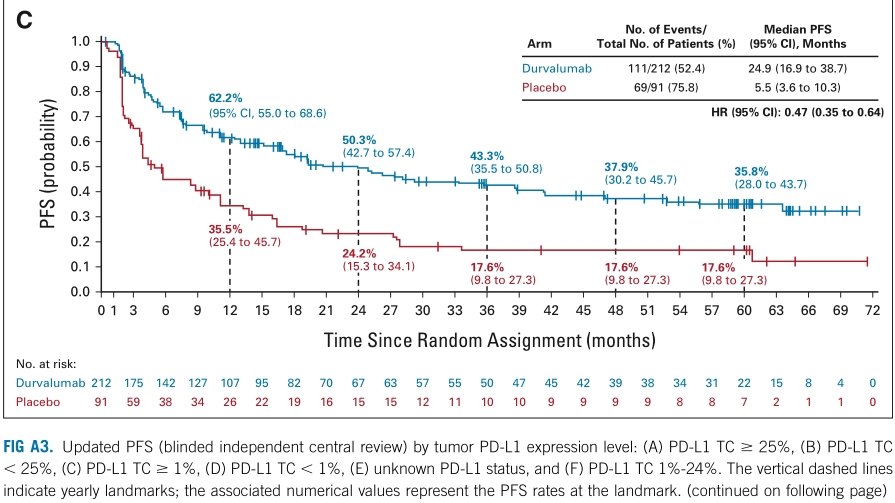
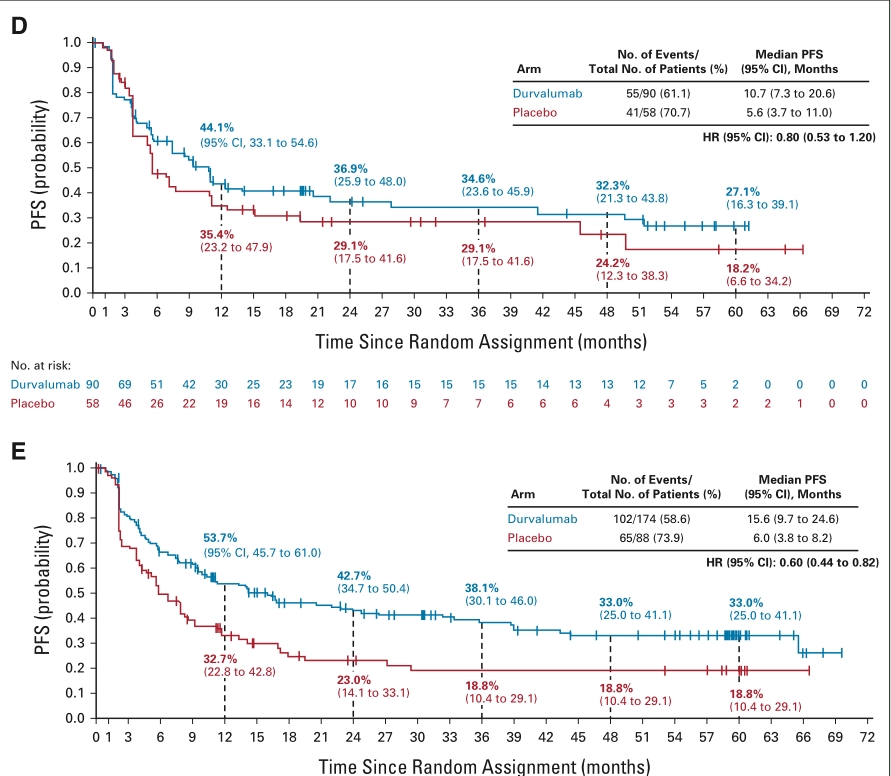
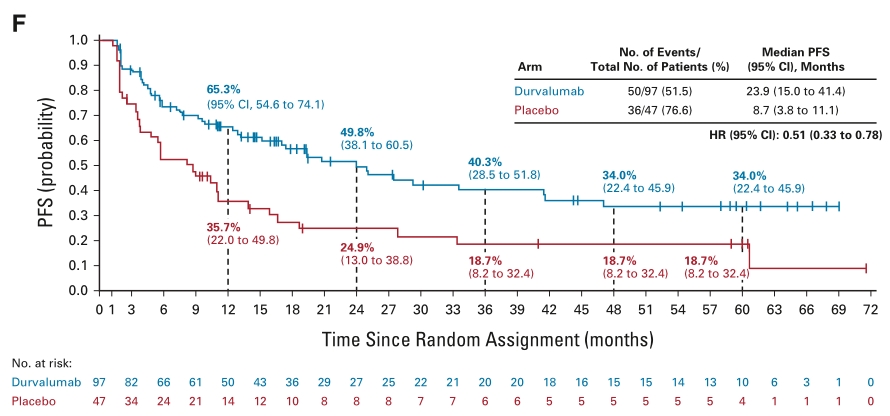
PD-L1 TC<1%患者中, durvalumab和安慰剂组的中位PFS分别为10.7 (7.3 to 20.6)和5.6 (3.7 to 11.0)个月(HR (95% CI): 0.80 (0.53 to 1.20)); PD-L1不明患者中, durvalumab和安慰剂组的中位PFS分别为15.6 (9.7 to 24.6)和6.0 (3.8 to 8.2)个月(HR (95% CI): 0.60 (0.44 to 0.82)); PD-L1 TC 1%-24%患者中, durvalumab和安慰剂组的中位PFS分别为23.9 (15.0 to 41.4)和8.7 (3.8 to 11.1)(HR (95% CI): 0.51 (0.33 to 0.78))。
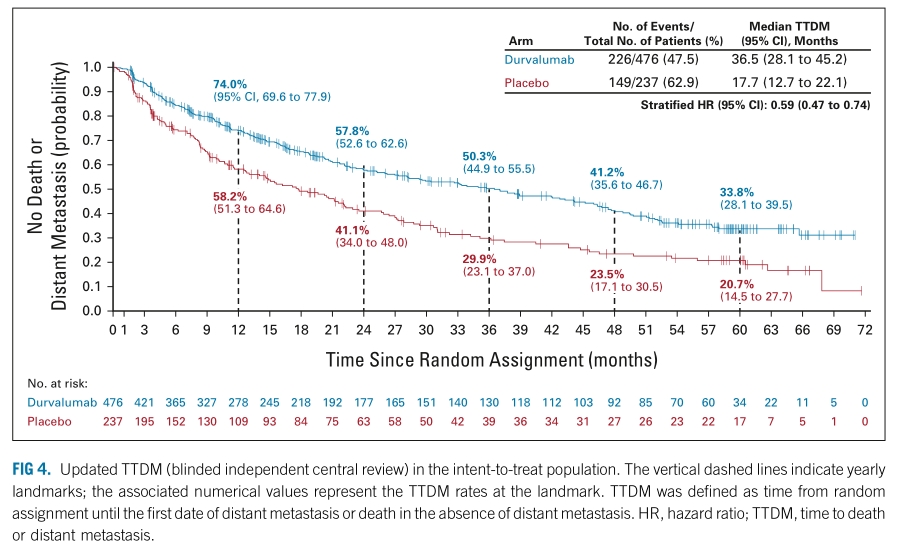
Durvalumab组的中位TTDM(随机化开始至第一次远处转移或死亡的时间)为36.5 (28.1 to 45.2)个月,安慰剂组为17.7 (12.7 to 22.1)个月( HR (95% CI): 0.59 (0.47 to 0.74))。
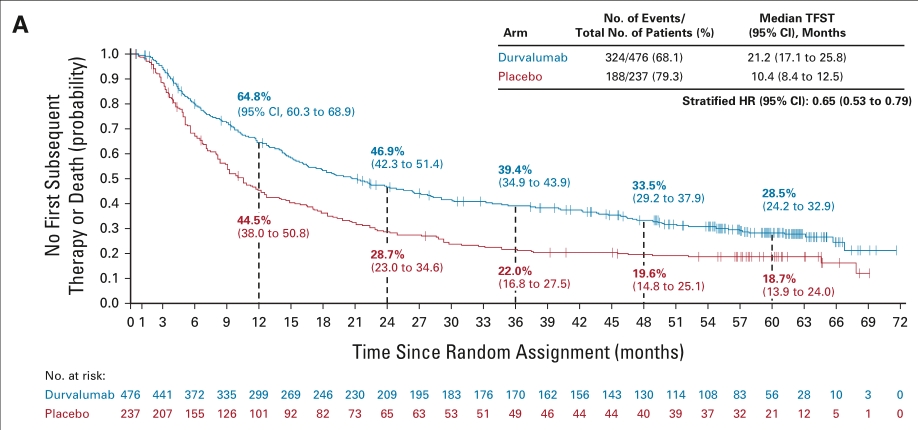
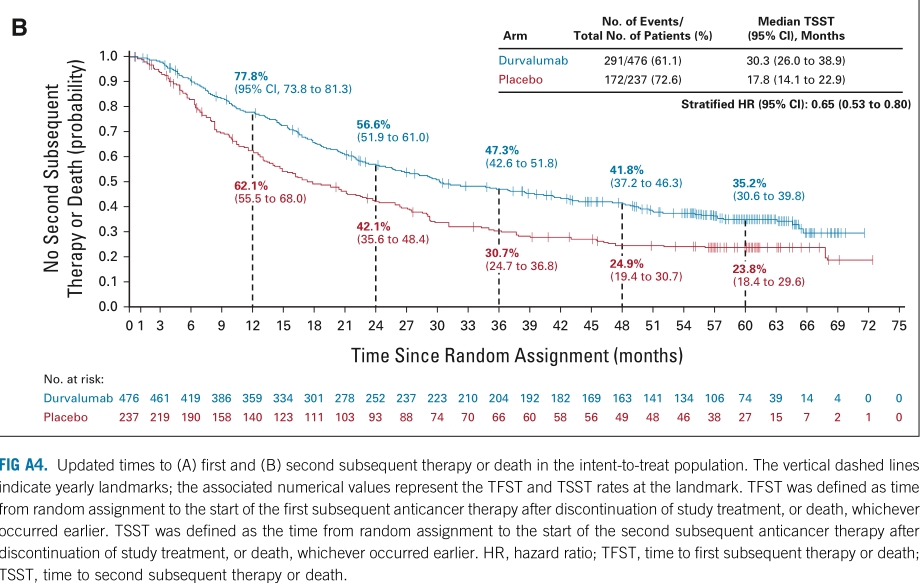
Durvalumab组的中位 TFST(随机化开始至第一次后线抗肿瘤治疗或死亡的时间)为21.2 (17.1 to 25.8)个月,安慰剂组为10.4 (8.4 to 12.5)个月( HR (95% CI): 0.65 (0.53 to 0.79)); Durvalumab组的中位 TSST(随机化开始至第二次后线抗肿瘤治疗或死亡的时间)为30.3 (26.0 to 38.9)个月,安慰剂组为17.8 (14.1 to 22.9)个月( HR (95% CI): 0.65 (0.53 to 0.80))。
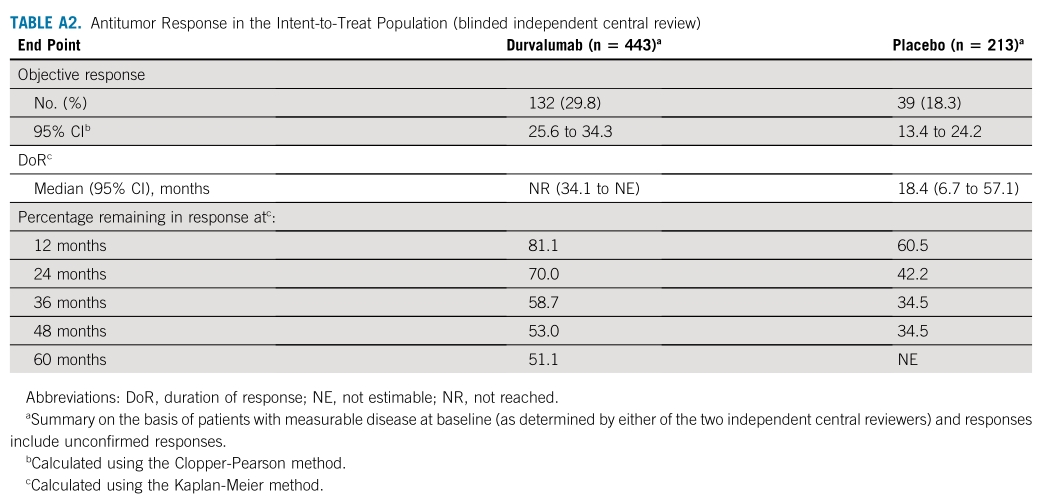
Durvalumab组的ORR为29.8%,安慰剂组为18.3%。
综上,PACIFIC研究5年生存结果提示放化疗后durvalumab(德瓦鲁单抗)持续改善III期NSCLC患者的预后。
原始出处:
David R. Spigel, Corinne Faivre-Finn, Jhanelle E. Gray, et al. Five-Year Survival Outcomes From the PACIFIC Trial:Durvalumab After Chemoradiotherapy in Stage III Non–Small-Cell Lung Cancer. JCO.February 2,2022: DOI https://doi.org/10.1200/JCO.21.01308
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#SCLC患者#
38
#mAb#
26
#Oncol#
35
#PACIFIC#
38
#III#
43
#放化疗#
50
#PACIFIC研究#
42
#NSCLC患者#
38
#III期#
0
学习学习学习了
44