JCO:全国、多中心研究:儿童脑肿瘤患者治疗后早期内分泌紊乱的流行率和危险因素评估
2016-11-14 MedSci MedSci原创
JCO:全国、多中心研究:儿童脑肿瘤患者治疗后早期内分泌紊乱的流行率和危险因素评估
目的:
评估儿童脑肿瘤(CBT)患者治疗后早期内分泌紊乱的流行率和危险因素
试验方法及病人入组情况:
这个全国性的研究共入组了2002年至2012年间诊断的718名诊断为CBTS并且在诊断后存活了2年的患者,其中排除颅咽或垂体腺肿瘤患者。所有内分泌的的研究结果都是从患者诊断治疗和随访期间病例中收集。研究采用使用多变量逻辑回归统计法来研究人口统计学与肿瘤和治疗相关的影响因素之间的关系,同时研究了早期内分泌紊乱的流行率。
试验结果:
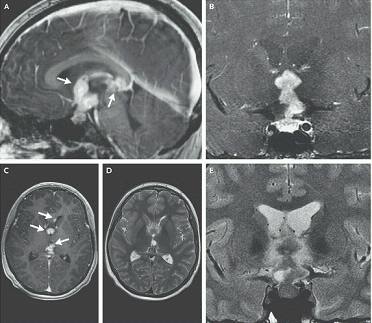
在中位随访6.6年后,有178例CBTS患者(24.8%)被诊断为内分泌紊乱。在治疗后的第一个5年中,共有159例CBT患者(22.1%)出现至少一种及以上内分泌紊乱现象。最常见的内分泌紊乱是生长激素缺乏(12.5%),青春期早熟(12.2%),甲状腺刺激激素缺乏(9.2%)和甲状腺功能减退(5.8%)。探究相关风险因素可发现,下丘脑 - 垂体功能障碍(n = 138)的风险与放疗(优势比[OR],15.74; 95%CI,8.72至28.42),诊断时年龄(OR,1.09;95%CI,1.04至1.14),进展随访时间(OR,1.10; 95%CI,1.02至1.18),脑积水诊断(OR,1.77; 95%CI,1.09至2.88)和蝶鞍上(OR,34.18; 95%CI,14.74至79.29)或腹膜内(OR,2.65; 95%CI,1.48至4.74)的肿瘤位点相关。
结论:
试验结果可以看到,CBT患者中出现早期内分泌紊乱疾病的流行率很高。随访患者中,共有22.1%例在治疗后的5年内出现至少一种以上内分泌紊乱现象。因此,尽早并定期评估高风险CBT患者的内分泌功能是十分有意义的。
原始出处:
Clement SC, Meeteren AYNS-v, Boot AM, Grinten HLC-vd, Granzen B, Han KS, et al. Prevalence and Risk Factors of Early Endocrine Disorders in Childhood Brain Tumor Survivors: A Nationwide, Multicenter Study. Journal of Clinical Oncology;0:JCO675025.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#分泌#
30
#流行率#
28
#内分泌紊乱#
31
#JCO#
30
#多中心研究#
33
#多中心#
31
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
93
讲的好,学习了
76
#脑肿瘤#
31
#肿瘤患者#
29