朱文玲:晕厥诊断与鉴别诊断新概念
2015-08-10 朱文玲 中国循环杂志
晕厥是临床上常见的症状,占急诊科患者的1%~1.5%,住院患者的1%~6%。导致晕厥的病因很多,机制复杂,涉及多个学科。晕厥预后从大多数的良性过程到少数患者的猝死后果差别很大,因此,在众多短暂意识丧失的患者中识别出晕厥患者并明确晕厥的分类至关重要。近年来,国际上对晕厥的评估有了一些新概念,强调从两方面评估晕厥患者:一是找出确切的原因,以便进行有效的针对病理机制的治疗;二是识别患者的风险,这种风
晕厥是临床上常见的症状,占急诊科患者的1%~1.5%,住院患者的1%~6%。导致晕厥的病因很多,机制复杂,涉及多个学科。晕厥预后从大多数的良性过程到少数患者的猝死后果差别很大,因此,在众多短暂意识丧失的患者中识别出晕厥患者并明确晕厥的分类至关重要。近年来,国际上对晕厥的评估有了一些新概念,强调从两方面评估晕厥患者:一是找出确切的原因,以便进行有效的针对病理机制的治疗;二是识别患者的风险,这种风险常取决于潜在的疾病而不是晕厥本身。
短暂意识丧失(T-LOC)包括各种机制导致的、以自限性意识丧失为特征的所有临床病症,而晕厥是T-LOC的一种形式(图1)。晕厥指由于短暂的全脑组织缺血导致的T-LOC,特点为发生迅速、短暂、自限性、并能够完全恢复的意识丧失。满足这4个特点的T-LOC为晕厥。
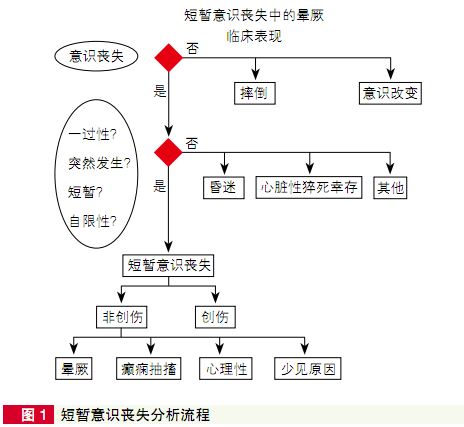
晕厥鉴别诊断的一个重要内容是癫痫发作,癫痫可引起T-LOC,患者无反应、摔倒、然后遗忘,这种情况仅在强直、阵挛、强直一阵挛及全身发作时出现。在儿童失神发作和成人部分复杂癫痫表现为意识的变化,而不是丧失。
无意识过程中身体完全松弛不支持癫痫,唯一的例外是“松弛发作”,但很少见。儿童伴预先存在神经系统疾病者可无诱因。癫痫和晕厥发作均可伴肢体运动。癫痫的运动可持续一分钟以上,晕厥持续数秒钟。癫痫发作时的抽搐粗大,有节奏,一般是同步的,而晕厥发作一般是非同步、幅度小而无节奏。但是,同步阵挛也可发生在晕厥患者。晕厥患者的痉挛运动仅发生在意识丧失出现后及摔倒后,而癫痫患者则不同。
晕厥通常有诱因,癫痫则少有诱因。反射性癫痫的诱因如闪光与晕厥不同。典型的癫痫先兆包括腹部感觉异常和(或)罕见的不愉快的气味。感觉异常在晕厥患者少有发生。癫痫发作常发生咬舌,一般位于舌的侧面,而晕厥一般在舌尖。两者均可发生尿失禁。癫痫发作后患者可能会较长时间处于混乱状态,而晕厥发作后患者一般会立即头脑清醒(表1)。癫痫发作后常出现头痛、肌肉痛、肌酸激酶和催乳素升高。
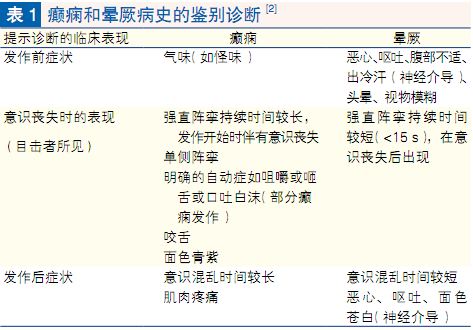
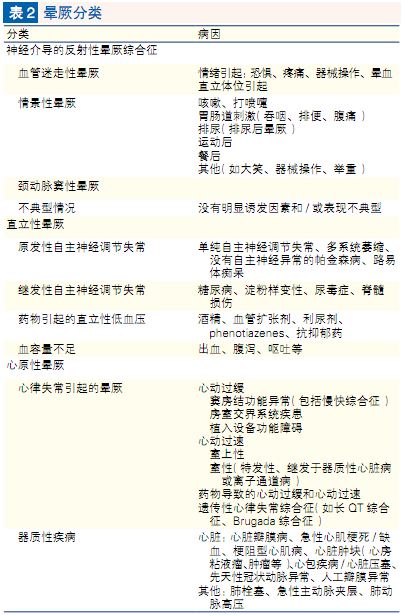
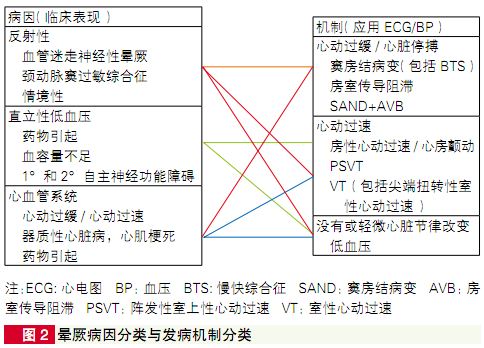
表2列出了基于主要病因和病理生理的晕厥分类,强调晕厥表现相同但风险不同。病理生理特点是体循环血压下降伴脑血流减少,是晕厥的发病基础。脑血流中断6~8秒就足以引起完全的LOC。倾斜试验的经验显示收缩压专60mmHg就会引起晕厥。收缩压由心输出量(CO)和总的外周血管阻力决定,任何一方面的减低都会引起晕厥,二者经常同时存在,只是作用大小不同。
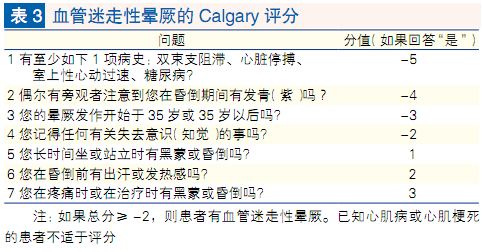
目前国际上应用Calgary评分(Calgary Score)诊断VV,包括7个有关病史、触发因素、环境、T-LOC的征象和症状的问题(表3)。所有问题均回答为“是”或“否”。如果一个问题回答为“是”,则根据答案是否增加VVS的可能性而加分或减分。每个问题的分值相加得到总分(范围:-14至+6分)。如果总分为-2或大于-2,则诊断VVSc。Calgary评分诊断VVS的敏感性为87%(95%CI:82%~91%),特异性为32%(95%CI:24%~40%)。
对于T-LOC疑似晕厥的患者需要初步评估,有必要时需要再评估。通过初步评估约23%~50%的晕厥患者的病因可明确,对于原因不明的患者重要的是危险分层。晕厥诊断流程见图3。
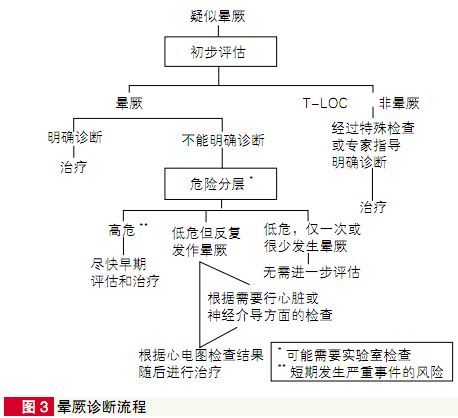
初步评估包括详细询问病史、体格检查(包括测量不同体位血压)、心电图。在此基础上,可适当增加其他检查以保证诊断准确:①40岁以上患者建议首先进行颈动脉窦按摩(但国内很少做);②对于有心脏病病史或怀疑此次晕厥与结构性心脏病或其他心血管疾病有关的患者,建议进行超声心动检查;③对于怀疑因心律失常而导致晕厥的患者,应给予实时心电监测;④若晕厥与体位变化有关或怀疑反射性晕厥时,则应进行相关检查。如卧立位试验和(或)直立倾斜试验等;⑤仅在怀疑非晕厥原因造成的短暂意识丧失的情况下,进行神经科检查或血液检查。
初步评估应明确以下三个关键问题:①是否为晕厥发作?②是否可确定晕厥的病因?③是否有证据表明患者为心血管疾病高危患者?
3.2 病因诊断
经过初步评估,约23%~50%的晕厥患者的病因可明确。表4列出初步评估后对诊断有意义的临床特征。

3.3 危险分层
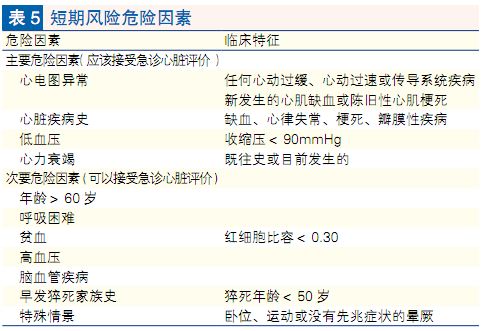
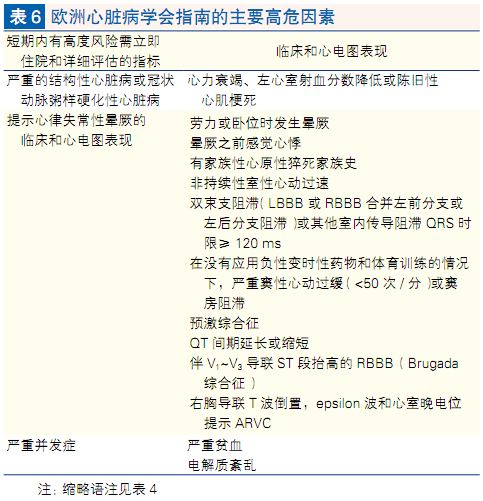
当初步评估后尚无法明确晕厥原因时,需立即进行主要心血管事件及心原性猝死风险的评估。近期风险(7~30天):晕厥后近期内出现危及生命事件风险的患者应住院诊治。加拿大心血管病学会2011发表的评估晕厥标准方案的学会声明中指出了短期危险因素(表5)。主要危险因素指多个研究报道的独立危险因素,次要危险因素指一个研究报道的危险因素。具备一个主要危险因素晕厥患者应紧急(2周内)心脏评估,具备一个或更多次要危险因素的患者也应考虑紧急心脏评估。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很好的东西,值得收藏~
137
#晕厥#
27
#鉴别诊断#
27
好东东
100
好好学习学习
102
刚刚有个朋友晕
94
总结的非常好
146