腰椎侧位图:

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
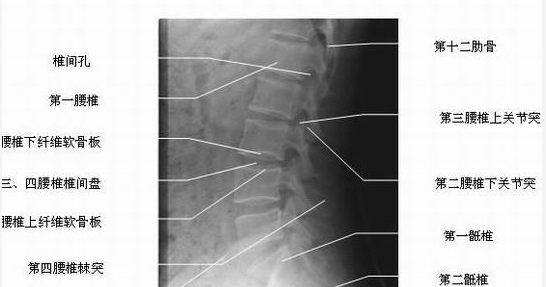
腰椎侧位图:


原标题:世界脊椎日来了,你知道哪节脊椎最易受伤?10月16日是世界脊椎日,很多人可能不知道人一共有多少块脊椎,但对脊椎病却熟悉得不能再熟悉了,因为颈椎痛、腰痛,甚至是由此带来的头痛、腿痛,每天都在困扰着大部分人。据统计,全球范围内,美国每年被脊椎病缠身的人约有540万;英国平均每1000名男性中,每年因此病不能工作的天数为627天,女性为347天。在中国,80%左右的人都不同程度地有过腰痛或腿痛的
腰椎融合术为处理众多脊柱退变性疾病的常规方法。腰椎融合术的总体并发症发生率高达13%。腰椎融合术并发症发生率与危险因素之间的相关性仍为当今研究的焦点。然而,没有研究深入地探讨脊柱外科专业对腰椎融合短期并发症发生率(术后1月)的影响。为了评价骨科专业、神经外科专业与单节段腰椎融合术后短期并发症发生率(术后1月)的相关性,美国学者Kim等进行了一项回顾性配对研究,该研究结果已在近期的Spine杂志上发
黄韧带起于颈2椎体,沿脊柱,终于骶1。在相邻的椎板间走行,黄韧带构成脊柱椎管的背侧表明。对黄韧带经典的解剖描述由Naffzinger等于1938年提出,在他们的描述中,黄韧带起于上位椎板的下方或前下方,止于下位椎板的上方或后上方。 后续有学者将其分作棘突间、椎板间和关节囊间三部分,进而分为浅层和深层两部分。但迄今为止,关于黄韧带在椎管外侧的大体解剖研究很少。深入研究其解剖特点,有利于放射科医生和
腰椎退变疾病寻求手术治疗的患者,功能受限和残障常为主诉,严重影响他们参加正常工作和娱乐,进而导致生产力下降,社会参与程度低,影响生活质量。腰椎管狭窄常伴有神经源性间歇性跛行,活动时加剧,伴有下肢麻木、无力和疼痛。从而导致活动受限和腰痛。 脊柱外科医生常关注患者为中心的疼痛、功能和残障结果。但此三者间的相互作用,尚不明确。 美国约翰霍普金斯大学骨科的学者,进行了一项前瞻性队列研究,提示腰椎术后3
腰椎椎间盘切除手术的目的是减缓疼痛,但手术本身可导致术后疼痛。绝大多数患者经历术后腰痛,导致术后住院时间延长和恢复正常活动时间延迟。为减轻术后疼痛,不得不使用麻醉药或止痛药,可致并发症,包括谵妄,恶心,呕吐,呼吸抑制等。因此,减少术后使用麻醉药或止痛药就很必要。 利多卡因是众所周知的局麻药,在某些病例具有抗炎和抗缺血效应。另外,术后疼痛与多种机制有关,包括痛觉敏感,炎症,肌肉痉挛,肠道胀气和组织
椎体软骨终板分为骨性终板和软骨终板,其作用非常重要,对维持脊柱的整体以及椎间盘的功能有重要的意义,研究表明终板的生物力学和生物化学特性的改变容易引起椎间盘退变相关疾病。腰椎终板及终板下骨质在MRI上的信号改变被称为Modic改变,其发生率正常人群中为6%,腰背痛人群中为40%,Modic改变在中年会进展,而且具有一定的遗传易感性。伴有Modic改变更容易影响腰痛患者的工作和生活。因此Modic


梅斯医学MedSci APP
医路相伴,成就大医
收藏
87
好文章,值得收藏
111
好文章,值得收藏
51
#腰椎#
37
#X线#
27