一、非小细胞肺癌CT定位前准备
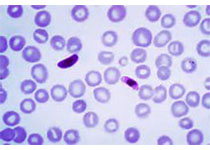
患者定位1周前病灶内已置入金标。
患者行放射外科治疗定位使用体垫或者胸网固定。
尽量使用增强CT扫描定位。
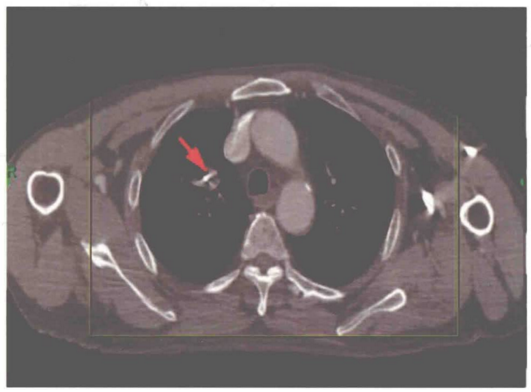
置入金标示意图
二、CT定位要求
1. 患者体位:仰卧位,双侧上肢置于身体两侧或抱头。
2. 呼吸时相:自由呼吸呼气末。
3. 扫描层厚:1.5mm.
4. 扫描范围:病灶上、下15cm.
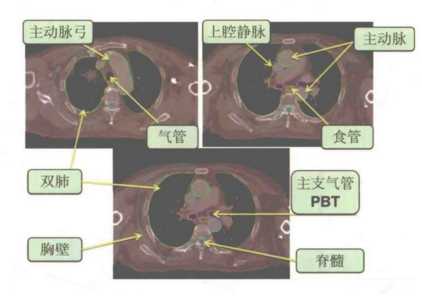
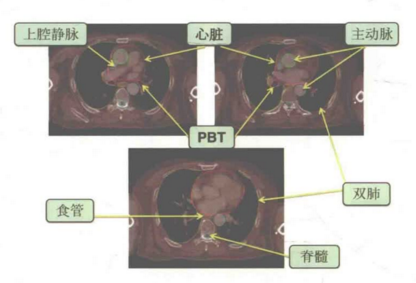
三、非小细胞肺癌放射外科勾画的正常器官
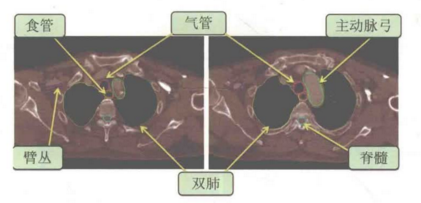
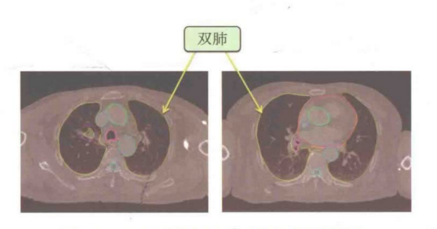
双肺
1. 在肺窗下勾画双肺。
2. 所有炎症、纤维化和不张的肺都应勾画在内,肺门区小血管也应包括在内。
3. 气管/支气管、GTV不应包含其中。
4. PET/CT有助于辨别肺不涨与GTV。
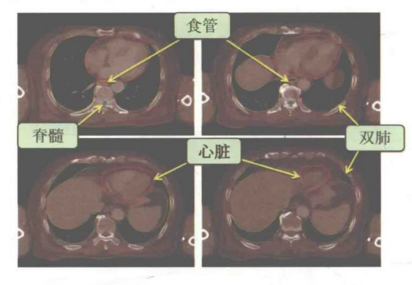
食管
1. 在纵隔窗下勾画食管。
2. 包括黏膜、黏膜下、肌层至脂肪外膜。
3. 范围:PTV上下10cm(超过环状软骨和食管胃连接部则终止于这些结构)。
近端支气管树(PBT)
1. 在纵隔窗下勾画PBT。
2. 范围:近端2cm的气管,隆突,主支气管,右侧上、中、下叶支气管,左侧上、下叶及舌段支气管。
3. 包括这些结构相应的黏膜、黏膜下层、软骨环和气道。
气管
1. 在纵隔窗下勾画气管。
2. 包括黏膜、黏膜下层、软骨环和气道。
3. 范围:PTV上10cm或隆突上5cm(两者取更靠上的)。
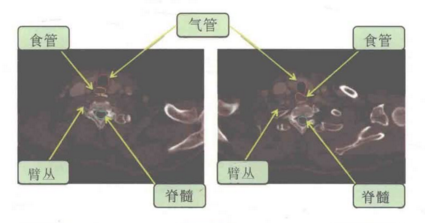
脊髓
1. 按骨髓腔的骨性标志勾画脊髓。
2. 范围:PTV上、下10cm(超过颅底和L2则终止于这些结构)。
臂丛
1. 病灶位于上叶,患者需要勾画臂丛,只需勾画同侧即可。
2. 范围:C4-C5到T1-T2水平神经孔的脊髓神经,到锁骨下血管神经束终止。(备注:没有神经孔的水平,勾画前、中斜角肌之间德间隙或软组织。)
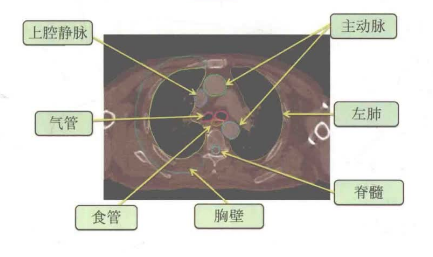
心脏和血管
1. 在纵隔窗下,心脏沿着包裹勾画,血管包全血管壁肌层至脂肪外膜。
2. 血管:右侧病灶勾画上腔静脉,左侧病灶勾画主动脉。
3. 范围:心脏勾画从肺动脉经过中线层面开始至心尖部,血管勾画PTV上、下10cm.
胸壁
1. 通过同侧肺在外侧、后侧及前方各自动外扩2cm生成。
2. 范围:前内侧到胸骨边缘,后内侧到椎体包括脊神经根出现德部位:PTV上、下3cm.
3. 建议靠近胸壁德病灶,勾画胸壁。
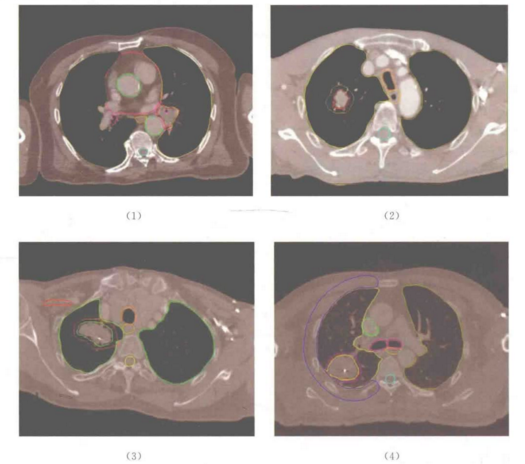
四、非小细胞肺癌示例:靶区及危及器官勾画
五、非小细胞肺癌放射外科治疗剂量建议
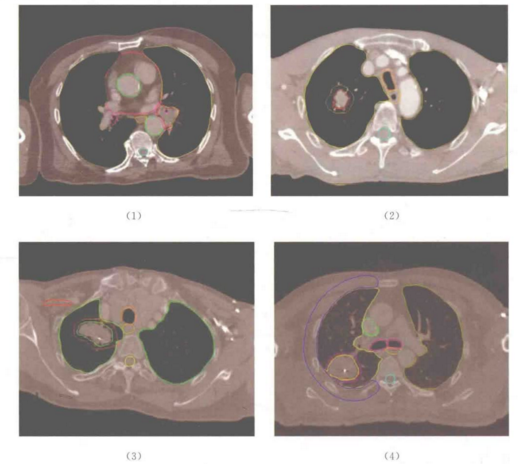
注:(1)位于肺门66Gy/8次;(2)周围型60Gy/3次;(3)临近臂丛60Gy/6次;(4)贴近胸壁60Gy/5次
参考文献:
[1]袁双虎,宋启斌主编.肿瘤精准放疗靶区勾画图谱[M].武汉:湖北科学技术出版社.2018.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#靶区勾画#
42
#非小细胞#
27
#靶区#
46
认真学习了。
68