ARD:抗纤维化因子KLF4在真皮成纤维细胞中被miR-10/TFAP2A/TBX5轴抑制
2022-01-20 网络 网络
KLF4在系统性硬化症(SSc)的皮肤成纤维细胞中具有抗纤维化作用,其表达受到TmiR-10/TFAP2A/TBX5轴的抑制。
背景:系统性硬化症(SSc)是一种病因不明的复杂疾病,其中炎症和纤维化导致多器官损伤。目前还没有有效的治疗方法可以阻止或逆转纤维化的进展,因此迫切需要对疾病发病机制提供新见解并确定新的潜在治疗靶点的研究。SSc双胞胎的疾病一致性较低,暗示表观遗传学在疾病中的作用。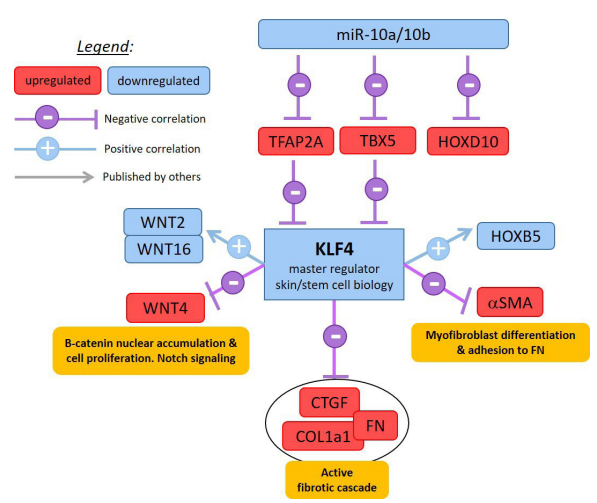
方法:研究者使用来自与SSc不一致的独特双胞胎队列(15对)的皮肤成纤维细胞(dFB)的全局基因表达(RNA-seq)和全基因组DNA甲基化分析来识别这种疾病的病理学分子特征。研究者使用体外、离体和体内模型验证了这些发现。
结果:该研究揭示了不同的差异表达和甲基化基因,包括参与干细胞分化和发育程序的几种转录因子(KLF4、TBX5、TFAP2A和HOXB3、HOXB8等同源框基因)。HOX基因抑制microRNA10a/10b的表达。miR10a位于17号染色体上HOXB4 的上游,而miR10b位于2号染色体上HOXD4的上游。对SSc患者皮肤成纤维细胞的两种microRNA 的分析显示这些microRNA水平降低。因此,microRNA10a/10b的靶向基因TFAP2A和TBX5 在这双胞胎队列中确实上调了。正常真皮成纤维细胞中miR10a 和miR10b的沉默导致 TFAP2A和TBX5的mRNA上调。在SSc成纤维细胞中恢复正常水平的miR10a 和10b 可使 TFAP2A和TBX5的表达正常化,并降低I型胶原蛋白的异常表达。研究者继续检查胚胎干细胞转录因子,发现SRY-box 2 (SOX2) 表达增强和KLF4 表达降低,特别是在SSc的早期阶段。KLF4表达受到TBX5和TFAP2A的抑制。结果还表明KLF4具有抗纤维化作用,其在成纤维细胞中的条件性敲除促进了纤维化表型。
结论:该研究的数据支持表观遗传失调在介导dFBs中SSc易感性中的作用,说明 CpG甲基化、miRNA和转录因子在SSc发病机制中的复杂相互作用,并强调未来使用表观遗传修饰剂作为治疗的潜力。
出处:
Malaab M, Renaud L, Takamura N, et al. Antifibrotic factor KLF4 is repressed by the miR-10/TFAP2A/TBX5 axis in dermal fibroblasts: insights from twins discordant for systemic sclerosis. Annals of the Rheumatic Diseases 2022;81:268-277.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#FAP#
50
#miR#
51
#抗纤维化#
0
#成纤维细胞#
67
#纤维细胞#
65
#KLF4#
43
学习#学习#
55