Nature Medicine:激活小肠FXR,向肥胖说不!
2015-02-09 佚名 生物谷
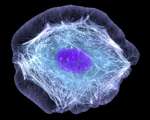
近日,著名国际期刊Nature Medicine发表了美国科学家的一项最新研究成果,他们发现特异性激活肠道FXR会促进肠道FGF15表达改变胆汁酸组成成分,同时能够通过增加产热以及白色脂肪棕色化,改善肥胖小鼠的体重及代谢恶化表型。 研究人员指出,目前利用胆汁酸感应因子FXR的全身性表达靶向胆固醇代谢,甘油三酯合成,肝脏脂肪变性和胆汁淤积治疗相关疾病正成为新兴疗法。相比于全身性治疗
原始出处
Fang S1, Suh JM1, Reilly SM2, Yu E1, Osborn O3, Lackey D3, Yoshihara E1, Perino A4, Jacinto S1, Lukasheva Y1, Atkins AR1, Khvat A5, Schnabl B3, Yu RT1, Brenner DA3, Coulter S6, Liddle C6, Schoonjans K4, Olefsky JM3, Saltiel AR2, Downes M1, Evans RM7.Intestinal FXR agonism promotes adipose tissue browning and reduces obesity and insulin resistance.Nat Med. 2015 Feb
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CIN#
32
#Nat#
0
#DIC#
26
不错的文章,学习了
123
已阅
43
已阅
95
#Medicine#
32
#Med#
21
#FXR#
33