Cell Metab:重新定义肥胖与疾病的关系!科学家用多组学数据重新划分肥胖类型,并准确预每种胖究竟更容易患哪种病
2018-10-27 奇点糕 奇点网
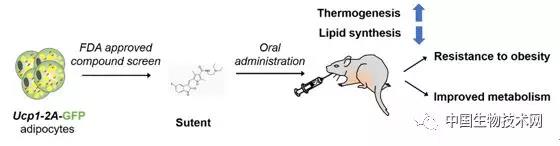
Scripps Research基因组学教授Amalio Telenti博士开始了一项大型研究,对BMI相关的代谢组和基因组进行了多组学分析,试图找到一个更准确的衡量肥胖的方法,对判断疾病的风险提供更精确的参考。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新定义#
49
#CEL#
41
#Cell#
34
#Meta#
44
#MET#
35
了解一下谢谢
80