人诱导多能干细胞分化为具有最小外源信号和部分转化为幼稚状态的下丘脑加压素神经元或可治疗中枢性尿崩症
2022-10-29 刘少飞 MedSci原创
本研究的目的是诱导从人类 家族性神经垂体尿崩症 (FNDI)疾病特异性 iPSC 分化为具有最小外源信号的 AVP 神经元,专注于人类 iPSC 和小鼠 iPSC 之间初始状态的差异。
下丘脑在维持生理平衡方面发挥着重要作用,其中之一是生成和分泌精氨酸加压素(AVP),它控制着水平衡。家族性神经垂体尿崩症 (FNDI) 的特点是下丘脑神经元的退化导致AVP分泌的逐渐减少。FNDI患者的AVP基因位点突变已被确认,这些突变大多位于编码AVP载体蛋白的区域,即神经蛋白II(NPII)。因此,该研究团队使用转基因技术得到了具有Cys98stop(以前称为Cys67stop)突变的FNDI小鼠,这种突变发生在FNDI患者身上,用于病理分析。
该研究团队在之前的研究中,使用Cys98stop-knock-in FNDI小鼠模型发现,突变蛋白在ER中的积累引起的内质网(ER)压力可能与FNDI病理有关。然而,还需要进一步的研究,包括使用人类患者模型,以研究FNDI的整体病理机制。人类的FNDI相关研究受到技术限制,因为下丘脑活检不能在活人身上进行,而且人类FNDI患者的AVP神经元损失只在尸检研究中报道过。因此,从人类FNDI特异性诱导多能干细胞(iPSCs)中提取的AVP神经元是一种有希望的人类模型,可用于病理分析和药物开发。
研究目的:
该团队诱导从人类 FNDI 疾病特异性 iPSC 分化为具有最小外源信号的 AVP 神经元,如前所述 miPSC。为了将最小的外源信号应用于人类 iPSC,该团队专注于人类 iPSC 和小鼠 iPSC 之间初始状态的差异。
小鼠体内模型研究表明,突变型 AVP 前激素的积累与 FNDI 病理有关。然而,在体内研究人类 FNDI 病理学在技术上具有挑战性。因此,需要开发体外人体模型。当外源性信号在体外分化的早期阶段被最小化时,小鼠胚胎干细胞 (ESCs)/诱导多能干细胞 (iPSCs) 分化为 AVP 神经元,而人类 ESCs/iPSCs 死亡。
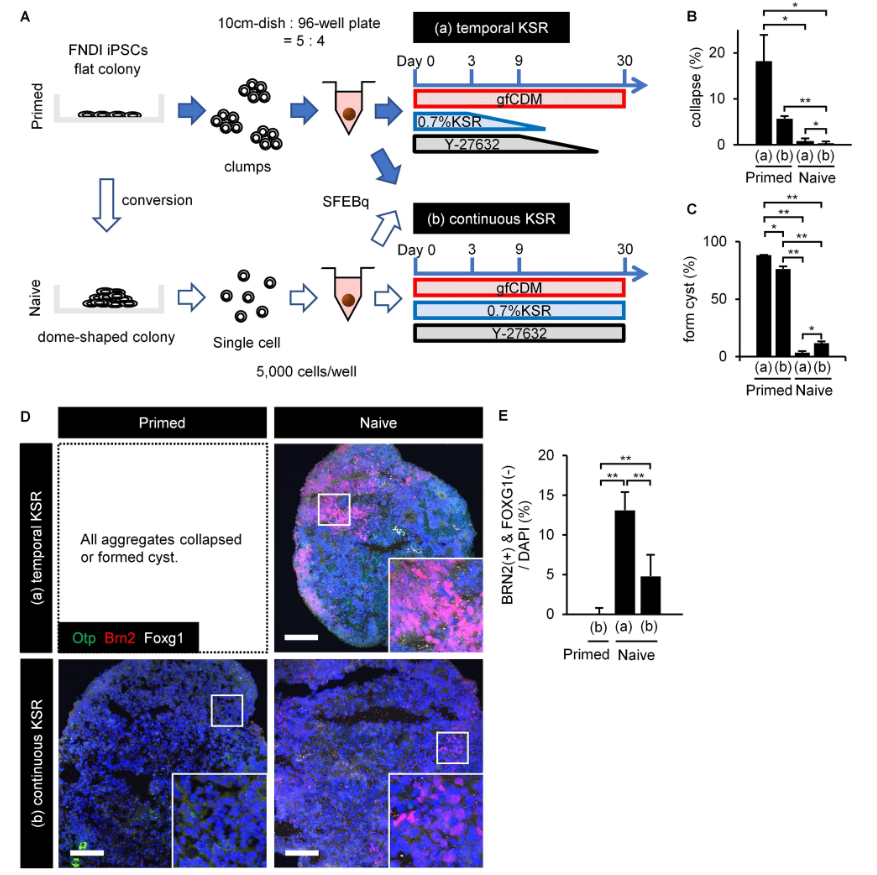
与小鼠 ESC 相比,人类 ESC/iPSC 通常更类似于小鼠外胚层干细胞 (mEpiSC)。在这项研究中,该研究团队通过naive conversion kit转换了人类 FNDI 特异性 iPSC。虽然转换是部分的,但该研究发现在最小的外源信号和分化为下丘脑喙部类器官的情况下,细胞存活率有所提高。总体而言,该方法提供了一个简单直接的分化方向,可以提高下丘脑分化的效率。
参考文献:
Ozaki H, Suga H, Sakakibara M, Soen M, Miyake N, Miwata T, Taga S, Nagai T, Kano M, Mitsumoto K, Miyata T, Kobayashi T, Sugiyama M, Onoue T, Takagi H, Hagiwara D, Iwama S, Banno R, Iguchi G, Takahashi Y, Muguruma K, Inoue H, Arima H. Differentiation of human induced pluripotent stem cells into hypothalamic vasopressin neurons with minimal exogenous signals and partial conversion to the naive state. Sci Rep. 2022 Oct 17;12(1):17381. doi: 10.1038/s41598-022-22405-8. PMID: 36253431; PMCID: PMC9576732.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









希望转化到临床应用
39
转发学习
34
感谢分享
38
学习受益
36