美国研发出癌症新疗法:用近红外线激活免疫细胞
2016-08-18 佚名 中国新闻网
据日媒报道,美国国立卫生研究院(NIH)主任研究员小林久隆等人在本月17日发行的美国医学杂志《科学转化医学》上发表研究成果称,开发出了通过近红外线照射激活攻击癌细胞的免疫细胞淋巴球来消灭癌细胞的疗法。 据称,通过小白鼠实验确认了该疗法对转移癌也有效。 报道称,淋巴球中有防止错误地攻击自身、发挥阻拦作用的细胞。癌症的免疫疗法会激活全身的淋巴球,因此存在着发生攻击健康细胞的“自身免疫反应”的风

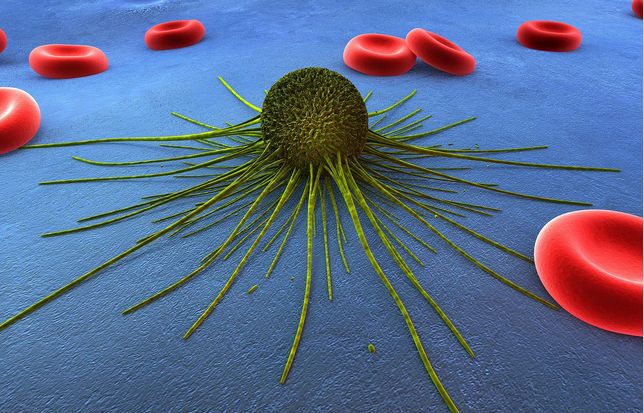
据日媒报道,美国国立卫生研究院(NIH)主任研究员小林久隆等人在本月17日发行的美国医学杂志《科学转化医学》上发表研究成果称,开发出了通过近红外线照射激活攻击癌细胞的免疫细胞淋巴球来消灭癌细胞的疗法。
据称,通过小白鼠实验确认了该疗法对转移癌也有效。
报道称,淋巴球中有防止错误地攻击自身、发挥阻拦作用的细胞。癌症的免疫疗法会激活全身的淋巴球,因此存在着发生攻击健康细胞的“自身免疫反应”的风险,但是减弱激活程度就会减弱治疗效果,这是尚未解决的难题。
而此次开发的疗法是仅破坏针对癌细胞的阻拦作用。小林称“有可能成为消除这一矛盾的强效药”。
小林等人使用了在特定波长的近红外线照射下会破坏周边细胞的化学物质,并将该物质和容易与发挥阻拦作用的“调节T细胞”结合的分子组合成了复合体。
将该复合体注射给移植了癌细胞的小白鼠,并仅在癌细胞上照射近红外线。结果显示,调节T细胞被破坏,激活了淋巴球,癌细胞减少,存活时间变长。
在将同一种癌细胞移植到不同部位、模拟转移癌的实验中,仅照射一个部位后,未照射的其他部位的癌细胞也减少了。分析认为,这是由于被照射的癌细胞内的淋巴球被激活后进入血液流向全身,并仅将特征相似的转移癌识别为攻击对象。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#近红外#
25
#红外线#
28
谢谢分享,学习了
44
有意思,好
33
很好,不错,以后会多学习
55
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
44
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
0
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
0
学习啦。。
32
如果可以,减少了多少病人的痛苦!
23