CORR:滑膜活检诊断髋关节假体感染准确率高
2013-06-09 CORR dxy
髋关节假体感染文献报道其发生率约1-3%,是髋关节置换术后最为严重的并发症,因此对关节置换术后存在髋关节假体松动或疼痛的患者术前准确的诊断是否存在感染非常重要。髋关节假体晚期感染和早期感染不同,有些患者并没有感染的典型临床表现,这给临床诊断带来了一定的困难。美国骨科医师协会(AAOS)工作组在其发布的一项指南中[美国感染协会PJI(假体感染)诊断及治疗指南]认为关节腔内抽液及CRP检查是诊断PJI
髋关节假体感染文献报道其发生率约1-3%,是髋关节置换术后最为严重的并发症,因此对关节置换术后存在髋关节假体松动或疼痛的患者术前准确的诊断是否存在感染非常重要。髋关节假体晚期感染和早期感染不同,有些患者并没有感染的典型临床表现,这给临床诊断带来了一定的困难。美国骨科医师协会(AAOS)工作组在其发布的一项指南中[美国感染协会PJI(假体感染)诊断及治疗指南]认为关节腔内抽液及CRP检查是诊断PJI的重要手段。关节腔内抽液可准确的进行细菌种类的鉴别和药物敏感性测验,同时可为一期或二期关节翻修时骨水泥中的抗生素填充提供指导。但目前文献报道其检测敏感性和特异性差别较大(如表1所示)。此前有文献报道术前膝关节假体滑膜活检较关节穿刺抽液和CRP敏感性好。尽管目前AAOS对PJI有相关的指导意见,但对何种方法最有效仍存在疑问,近日来自德国的临床医生就PJI检测方法的准确性进行对照研究,相关结论发表在CORR上。
表1:既往文献报道关节腔穿刺抽液细菌学培养准确率比较
研究者着重解决以下问题:1.在CRP,关节腔穿刺抽液,术中滑膜细菌学及组织病理学检测等三种方法中,何种方法最有诊断价值?2.单独应用上述诊断方法各自的诊断价值?3.联合应用上述诊断方法是否可以提高诊断的准确率?4.滑膜活检技术术后是否存在较高的并发症发生率?
改研究回顾性分析了2008年1月-2009年6月间就诊的100例因假体松动行髋关节假体翻修的患者数据。假体松动的定义依据Brand及Manaster标准(假体周围在随访过程中出现持续进展的透亮区域;在骨水泥-骨界面或金属-骨界面间出现>2mm的透亮线;骨水泥骨折;假体位置改变超过4mm或>4°)。
患者49例女性,51例男性,平均年龄68岁,93例患者关节置换术前诊断骨关节炎,7例患者诊断风湿性关节炎。最后一次术后距活检时间平均41月(4-312月),至少随访24月(平均32月,24-47月)。
所有患者在术前均检测CPR水平;根据Lonner等人的推荐,在关节腔穿刺抽液或滑膜活检前4周内禁止使用抗生素以减少抗生素诱导细菌培养假阳性的可能性。有3例患者术前存在置换部位的感染窦道,这些患者在活检术前也停止使用抗生素,每周检测感染指标,直至手术时。
关节穿刺抽液和活检在无菌条件下进行。若在同一部位不能抽出液体,则改换另一个部位,若仍无液体抽出,则向膝关节内灌注10ml生理盐水冲洗,留取冲洗的液体进行培养及检测;在C臂机透视下使用活检钳在滑膜线下及假体周围5个不同区域分别取2块不同组织进行细菌学及组织病理学检测。所有标本均在相同的特定培养基中进行细菌学培养。阴性定义为培养时间超过14天无细菌生长。
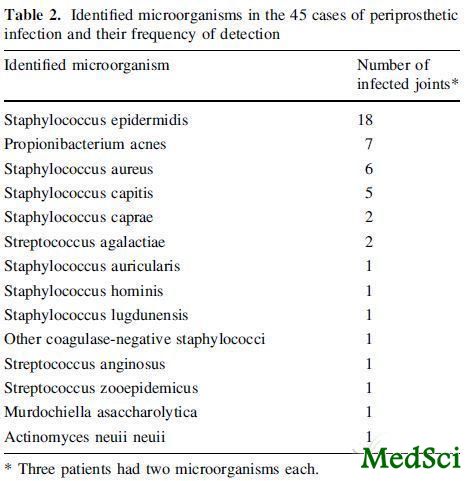
阳性及阴性定义:对活检标本,细菌学阳性定义为:两个或以上活检标本培养出至少一种相同类型的细菌;组织学阳性定义为:在10个高倍视野下(400×)至少发现一个视野内的多形核白细胞计数>5个;CRP值大于10mg/l定义为阳性。联合活检的细菌学和组织学检测结果,阳性为具备以下之一条件:在至少两个以上的标本中观察到同一种细菌;若只有一个细菌培养结果阳性,那么其他组织学检测中至少有一个结果阳性。除以上外的细菌结果阳性则认为是标本污染。关节假体部位是否存在感染最终取决于翻修术后患者大体滑膜标本检测及培养结果,最后结果显示,45例患者存在感染,55例患者无感染,42例患者最终培养分离出一种细菌标本,3例患者培养出两种标本,如表2所示。
表2:最终大体标本细菌培养结果阳性的细菌分布情况,其中表皮葡萄球菌为主要感染细菌
研究结果提示:
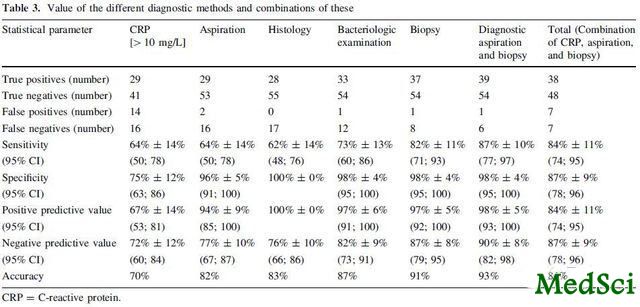
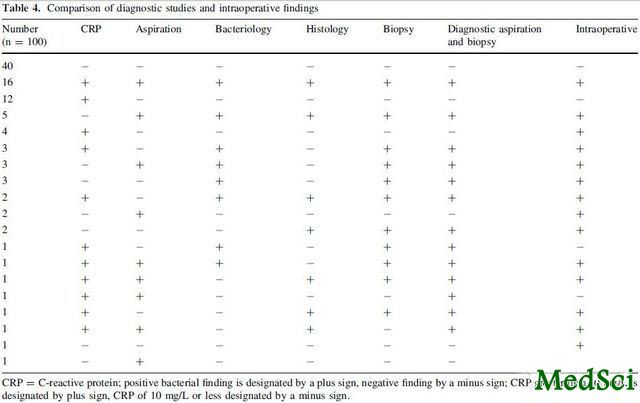
细菌学联合组织学的活检诊断准确率在三者中最高,敏感性82%,特异性98%,阳性预测率(PPV)97%,阴性预测率(NPV)87%,准确率91%;关节腔穿刺抽液其次,64%的敏感性,96%的特异性,阳性预测率(PPV)94%,阴性预测率(NPV)77%,准确率82%;CRP最差,64%的敏感性,75%的特异性,阳性预测率(PPV)67%,阴性预测率(NPV)72%,准确率70%;联合穿刺抽液和活检只能轻度提高诊断准确率,联合CPR和其他两种方法准确率无差异,最终结果如表3,4所示。术后未发现严重并发症。
表3:不同诊断方法的诊断准确率及联合诊断准确率
表4:诊断结果和最终结果比较
研究者分析实验数据得出以下结论:
1.本研究证实了膝关节滑膜活检术诊断感染具有较高准确率,但和膝关节不同,髋关节滑膜活检的有效性稍低,特别在敏感性及阴性预测率上。研究者认为这可能是由于膝关节活检取材方便,并具有广泛代表性,而髋关节受限于解剖结构,其取材范围只局限较少部位,不能完全代表关节内情况
2.和既往髋关节假体感染活检和穿刺抽液对比研究报道两者准确率不存在显著差异不同,本研究提示活检诊断关节假体感染更具优势,这可能是由于既往研究报道并未联合应用细菌学和组织学检测方法,并且在既往研究中,细菌培养时间较短,只有7天,而关节内感染的细菌生长较为缓慢,培养分离较困难,延长培养时间可以提高细菌检出成功率。
3.CRP和既往的文献报道相比,其准确率较低,可能是由于研究中纳入了风湿性关节炎患者,患者的CRP本身存在升高,影响了其准确性和特异性统计。
4.关节穿刺抽液细菌培养的准确率和既往文献报道相当。
在文章最后结论部分,研究者建议:髋关节滑膜活检术较关节腔穿刺抽液或CPR等方法诊断PJI准确性更高,对所有髋关节穿刺抽液培养阴性而CPR升高或存在感染临床征象的患者推荐滑膜活检优于重复穿刺抽液。

High diagnostic value of synovial biopsy in periprosthetic joint infection of the hip.
BACKGROUND
The role of the synovial biopsy in the preoperative diagnosis of a periprosthetic joint infection (PJI) of the hip has not been clearly defined.
QUESTIONS/PURPOSES
We asked whether the value of a biopsy for a PJI is greater than that of aspiration and C-reactive protein (CRP).
METHODS
Before revision in 100 hip endoprostheses, we obtained CRP values, aspirated the joint, and obtained five synovial biopsy samples for bacteriologic analysis and five for histologic analysis. Microbiologic and histologic analyses of the periprosthetic tissue during revision surgery were used to verify the results of the preoperative diagnostic methods. The minimum followup was 24 months (median 32; range, 24-47 months).
RESULTS
Forty-five of the 100 prostheses were identified as infected. The biopsy, with a combination of the bacteriologic and histologic examinations, showed the greatest diagnostic value of all the diagnostic procedures and led to a sensitivity of 82% (95% CI, ± 11%), specificity of 98% (95% CI, ± 4%), positive predictive value of 97% (95% CI, ± 5%), negative predictive value of 87% (95% CI, ± 8.3%), and accuracy of 91%.
CONCLUSIONS
The biopsy technique has a greater value than aspiration and CRP in the diagnosis of PJI of the hip (Masri et al. J Arthroplasty 22:72-78, 2007). In patients with a negative aspirate, but increased CRP or clinical signs of infection, we regard biopsy to be preferable to just repeating the aspiration.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









不错哦,学习了新知识!
54
#假体感染#
39
#活检#
50
#假体#
28
#ORR#
41