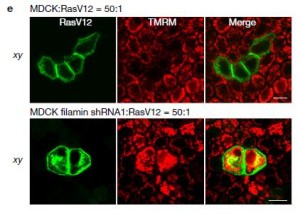
NAT COMMUN:肿瘤细胞恶化前会变“硬”
2017-07-12 佚名 生物通
乳腺癌的病程可能需要几个阶段,如最开始的良性和病变后的浸润癌,可能还会发生转移。只有20-50%的良性肿瘤最终会发展成为浸润癌。病变前的早期预测判断疾病的严重程度,从而选择相应的治疗手段。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#COMMUN#
30
#Nat#
34
学习了学习了学习了学习了学习了
73
#肿瘤细胞#
31
学习了谢谢分享
66
学习了分享了
70