Eur Heart J:直接PCI转运期间 比伐卢定优于肝素联合GPI
2014-06-09 高晓方 译 医学论坛网
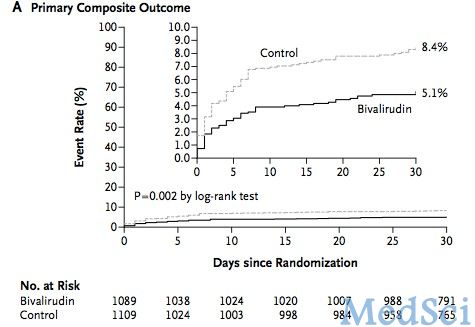
欧洲一项研究表明,与肝素联合常规和急救糖蛋白IIb/IIIa抑制剂(GPI)相比,比伐卢定均可降低心梗患者的大出血发生率,但同时可升高支架血栓形成发生率。论文5月21日在线发表于《欧洲心脏杂志》(Eur Heart J)。 此项研究共纳入2198例ST段抬高型心肌梗死患者,并在行直接PCI的转运期间给予比伐卢定或肝素联合可选GPI治疗。主要转归由30天时死亡或非CABG相关性大出血组成。对比伐卢
欧洲一项研究表明,与肝素联合常规和急救糖蛋白IIb/IIIa抑制剂(GPI)相比,比伐卢定均可降低心梗患者的大出血发生率,但同时可升高支架血栓形成发生率。论文5月21日在线发表于《欧洲心脏杂志》(Eur Heart J)。【原文下载】
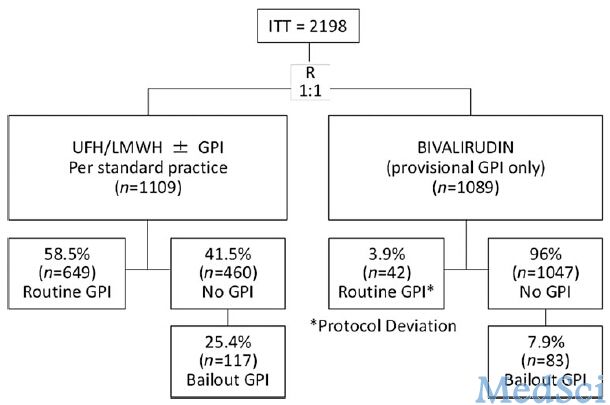
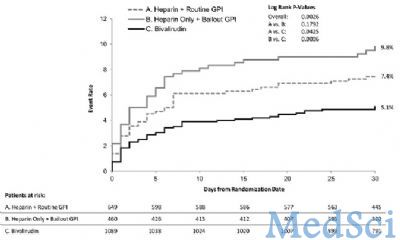
此项研究共纳入2198例ST段抬高型心肌梗死患者,并在行直接PCI的转运期间给予比伐卢定或肝素联合可选GPI治疗。主要转归由30天时死亡或非CABG相关性大出血组成。对比伐卢定组(1089例)、肝素联合常规GPI组(649例)和肝素联合仅急救期间给予GPI组的转归。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#转运期间#
22
#直接PCI#
39
#转运#
27
#比伐卢定#
40
#ART#
35
#HEART#
21