PNAS:颠覆 雌激素在宫颈癌癌中的作用
2015-06-12 生物通 生物通
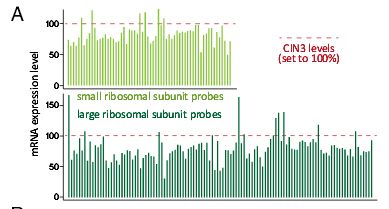
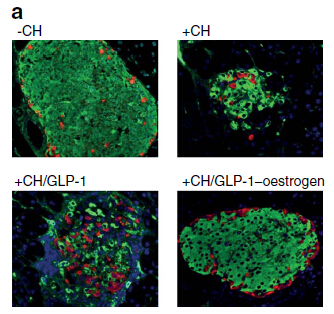
科学家们一直认为雌激素是宫颈癌生长的主要驱动因子。但一项最新研究表明,雌激素受体在宫颈癌细胞中几乎全部消失。相关论文发表在近期的美国国家科学院院刊PNAS杂志上。宫颈癌是女性中的第二大癌症,在发展中国家尤其常见,因为在那里早期筛查还不普遍。人们发现,几乎所有宫颈癌都是人乳头瘤病毒(HPV)感染引起的。研究人员对SUCCEED项目(Study to Understand Cervical Cance
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PNAS#
33
看看
124
?
112
#宫颈#
28
真是大师级的研究
98
?
112
?
107
这么说雌激素有可能不影响宫颈癌了!
92