J Clin Periodontol:釉质基质衍生物作为微创非手术治疗骨内缺损的辅助治疗手段
2022-03-28 MedSci原创 MedSci原创
骨内缺损在牙周病的进展和受累牙齿的长期脱落中发挥重要作用。然而,当进行牙周治疗后,再进行支持性的牙周治疗方案,就会阻止或显著减小疾病的发展。
骨内缺损在牙周病的进展和受累牙齿的长期脱落中发挥重要作用。然而,当进行牙周治疗后,再进行支持性的牙周治疗方案,就会阻止或显著减小疾病的发展。近日,发表于J Clin Periodontol的一项随机试验比较了微创非手术技术(MINST)联合或不联合釉质基质衍生物(EMD)治疗骨内缺损≤7毫米的疗效。
研究共纳入36名患者,随机分配到两组:对照组接受MINST,而实验组接受MINST+EMD。在基线、6个月和12个月时记录临床测量结果,在基线和12个月时进行影像学测量。
结果,所有受试者都完成了研究,每组18人。分析结果显示,两组受试者在12个月时都有明显的改善(p < .001),MINST组和MINST+EMD组在平均PD减少(4.0 ± 1.4 vs. 4.2 ± 1.7 mm)、CAL增加(3.5 ± 1.4 vs. 3.4 ± 1.6 mm)和骨缺损恢复(1.9 ± 1.1 vs. 1.8 ± 0.9 mm)方面分别没有差异(p > .05)。应用EMD后,牙周骨缺损回复程度更高(PD≤4毫米且无BoP)的趋势(77.8% vs. 55.6%的部位),尤其是基线PD≤8毫米的部位(92.3% vs. 69.2%的部位),同时也带来复合结果成功数量的增加(61.1% vs. 44.4%的位点)。
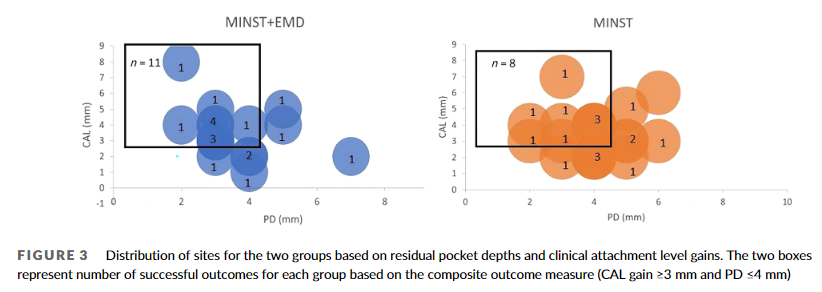
综上所述,该研究结果表明,MINST在治疗≤7毫米骨内缺损12个月后显示出明显的改善(包括临床和影像学结果)。额外应用EMD可增加牙周袋闭合度,特别是对于基线PD≤8毫米和骨内深度≤5毫米的位点,但并不能进一步改善平均临床或影像学结果。
原始出处:
Styliani Anoixiadou,et al., Enamel matrix derivative as an adjunct to minimally invasive non-surgical treatment of intrabony defects: A randomized clinical trial. J Clin Periodontol. 2022 Feb;49(2):134-143. doi: 10.1111/jcpe.13567.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#衍生物#
36
#基质#
34
#PE#
34
#手术治疗#
51
#微创#
31
#非手术治疗#
38