日本用iPS细胞治肾病初现曙光 肾透析或成历史
2015-03-17 佚名 中新网
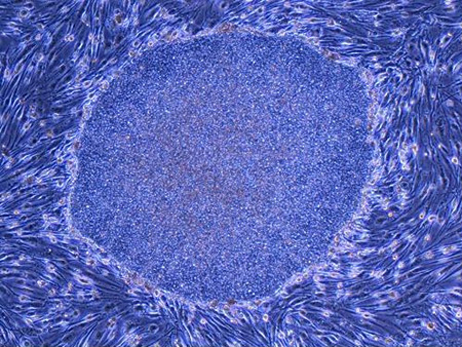
近日,日本一家大型制药公司和京都大学iPS细胞研究所展开合作,用iPS细胞制成的肾脏细胞成功治愈了急性肾功能不全这一重大疾病。若下一步研究能顺利进行,肾透析或将走入历史。 据报道,研究团队先将试验用小鼠的血管扎住,使之出现肾功能不全症状。然后,京都大学的长船健二教授等给小鼠移植了用人的iPS细胞制成的肾脏细胞。 试验发现,未经移植的小鼠出现了肾功能不全症状,而经移植的小鼠却没有。也就是说,
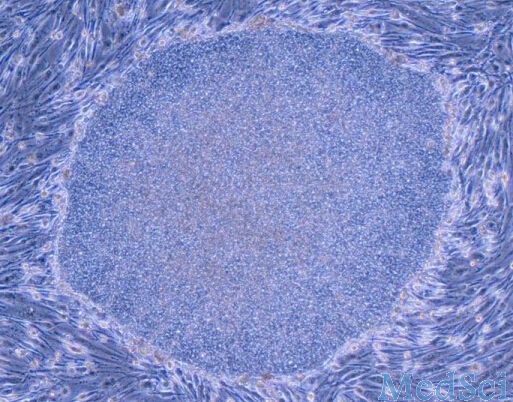
近日,日本一家大型制药公司和京都大学iPS细胞研究所展开合作,用iPS细胞制成的肾脏细胞成功治愈了急性肾功能不全这一重大疾病。若下一步研究能顺利进行,肾透析或将走入历史。 据报道,研究团队先将试验用小鼠的血管扎住,使之出现肾功能不全症状。然后,京都大学的长船健二教授等给小鼠移植了用人的iPS细胞制成的肾脏细胞。
试验发现,未经移植的小鼠出现了肾功能不全症状,而经移植的小鼠却没有。也就是说,用人类iPS细胞制成的肾脏细胞成功治愈了急性肾功能不全。
报道指出,虽然只是小鼠试验,却是研究人员首次用iPS细胞改善了肾功能不全的症状。研究团队希望通过其他动物试验来确认其安全性及有效性,力争在2025年以后开始临床研究。相关研究结果预计将于3月19日在横滨市举办的日本再生医疗学会上发表。
据了解,在肾功能不全方面,仅日本就有约30万患者,目前尚无根治方法。随着病情恶化,患者为去除体内的代谢产物需要接受人工透析,在给患者带来巨大不便的同时,医药费也相当昂贵。
报道称,虽然此次治疗的仅是急性肾功能不全,但京都大学的研究人员期待能进一步将其应用到治疗糖尿病、高血压等原因所引起的慢性肾功能不全上。
早在2014年秋季,日本理化学研究所等就实施了世界首例使用iPS细胞治疗眼部疾病的临床研究手术。此外,京都大学、大阪大学也将计划分别将该技术运用于帕金森病、心脏疾病的治疗上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#曙光#
37
#肾透析#
36
#日本#
45
#iPS#
34
#历史#
38
#iPS细胞#
38
好,但愿早日应用到临床
98
了
117