Medicine:亚洲人群COPD患者深静脉血栓的发生高于非COPD患者
2015-11-24 phylis 译 MedSci原创
大多数研究集中在高加索人慢性阻塞性肺疾病(COPD)患者深静脉血栓形成(DVT)及肺栓塞的发生及急性恶化。与高加索人群相比,亚洲人群发生DVT较少。这篇研究旨在探索亚洲COPD患者DVT的急性发生。研究者招募了1998年到2008年40岁以上的COPD(ICD-9: 490-492,496;A编码:A323和A325)患者。索引日期为第一次诊断为COPD的日期。研究者排除了在索引日期前患者COPD
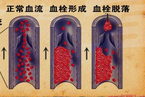
大多数的慢性阻塞性肺疾病(COPD)患者深静脉血栓形成(DVT)及肺栓塞的发生及急性恶化的研究集中在高加索人群中(又称欧罗巴人种、欧洲人种、欧亚人种、印欧人种或白色人种)。与高加索人群相比,亚洲人群发生DVT较少。这篇研究旨在探索亚洲COPD患者DVT的急性发生。
研究者招募了1998年到2008年40岁以上的COPD(ICD-9: 490-492,496;A编码:A323和A325)患者。索引日期为第一次诊断为COPD的日期。研究者排除了在索引日期前出现COPD和DVT(ICD-9-CM :453.8)的患者。按照年龄、性别及入院时间,以2:1设置对照组。从索引日期开始随访患者DVT的发生时、死亡发生时,直至2009年12月31号或者患者脱离了国家医疗保险计划时。COPD患者DVT的发生率为18.78/10000人每年,校正年龄、性别、房颤、高血压、糖尿病、高脂血症及脑血管事件、充血性心衰、下肢骨折或手术及癌症后,COPD患者发生DVT的校正HR值为1.38(95%CI:1.06-1.80),高于非COPD患者。
亚洲人群中,慢性阻塞性肺疾病(COPD)患者深静脉血栓形成(DVT)的发病率高于非COPD患者。
原文出处:
Chen CY, Liao KM. The Incidence of Deep Vein Thrombosis in Asian Patients With Chronic Obstructive Pulmonary Disease. Medicine. 2015 Nov
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










好文章
61
学习下,好
71
继续关注
48
#静脉#
37
#DIC#
21
亚洲人还有这种风险,希望做进一步研究
54
继续学习
50
继续关注
26
#CIN#
26
#静脉血#
18