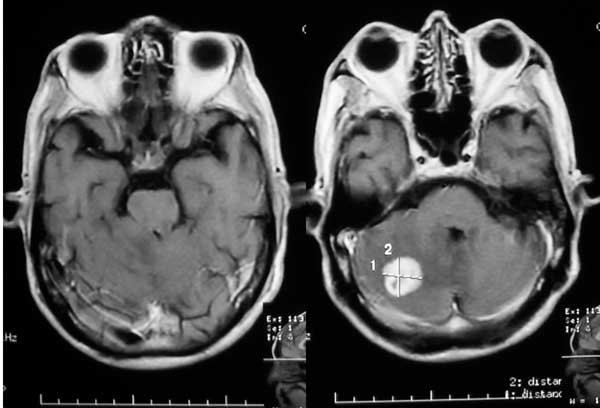
[脑转移]立体定向还是全脑放疗?看看临床医生交出的答卷
2017-03-15 Roxanne Nelson Medscape.com.
转移的治疗在过去的十年间有所进步,立体定向放射治疗(SRS)的使用越来越多。部分专家对于其是否能代替全脑放疗(WBRT)作为脑转移的标准治疗,仍存在争议。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#立体定向#
30
#定向#
31
#全脑放疗#
31
#临床医生#
32
没有临床研究来证实哪种方法更能获益
75
看看了解一下
55
文章不错,值得分享
56
Xox you
63