Neurosurgery:椎间孔镜微创治疗骨性椎间孔狭窄
2014-05-09 佚名 丁香园
腰椎间孔或侧隐窝狭窄的传统手术方法,可以归类为伴随或不伴随骨融合的全椎骨关节面切除术,和保持小关节的显微椎间孔切开减压术。全椎骨关节面切除术往往导致脊柱节段性不稳定和背痛。随着微创技术的发展,多位作者已经报告过,使用内窥镜技术来治疗腰椎间孔狭窄,但是这些技术的实际应用,都受限于柔软的椎间盘突出症。【原文下载】 韩国首尔的我立德脊柱医院神经外科的Yong Ahn博士进行了一项研究,提示局麻下经
腰椎间孔或侧隐窝狭窄的传统手术方法,可以归类为伴随或不伴随骨融合的全椎骨关节面切除术,和保持小关节的显微椎间孔切开减压术。全椎骨关节面切除术往往导致脊柱节段性不稳定和背痛。随着微创技术的发展,多位作者已经报告过,使用内窥镜技术来治疗腰椎间孔狭窄,但是这些技术的实际应用,都受限于柔软的椎间盘突出症。【原文下载】
韩国首尔的我立德脊柱医院神经外科的Yong Ahn博士进行了一项研究,提示局麻下经皮穿刺内窥镜下腰椎间孔切开减压术,是治疗骨性椎间孔狭窄的一个有效的手术方法,文章最近发表在Neurosurgery上。
该研究的目的是,描述适用于骨性椎间孔狭窄的、经皮穿刺内窥镜下腰椎间孔切开减压术这项技术的详细信息,同时阐述其临床效果。该研究是一项持续2年的前瞻性研究,纳入了连续的33例腰椎椎间孔狭窄患者,这些患者都接受了内窥镜下腰椎间孔切开减压术。
手术效果的评估,使用疼痛视觉模拟评分法(VAS)、 Oswestry功能障碍指数(ODI)和改良MacNab标准。手术过程开始于更安全的椎间孔外侧区域,而不是风险较高的椎间孔内侧区域。然后,可以使用内镜钻和微型钳在内镜控制下实行全面的椎间孔减压。

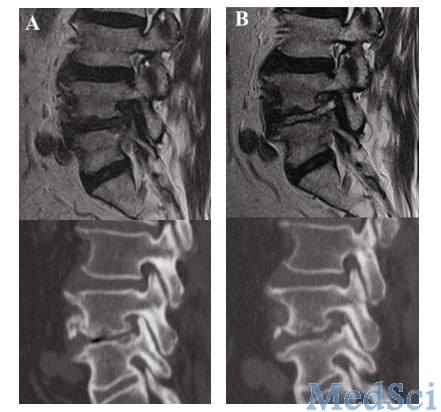
研究结果提示,局麻下经皮穿刺内窥镜下腰椎间孔切开减压术,可能是治疗椎间孔狭窄的一个有效的手术方法。特别是对于老年人或合并基础内科疾病的患者,此手术方法可以提供安全的和可重复的临床结局。这项手术技术的临床可行性非常大,逐渐成为标准化治疗,值得进一步推广使用。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#GER#
23
#微创治疗#
37
#椎间孔#
38
#椎间孔镜#
33
#surgery#
28
#微创#
25
#ROS#
29