JACC:冠脉支架植入后DAPT疗程不同 死亡率有何差异?
2017-05-04 闫盈盈;吴星 环球医学
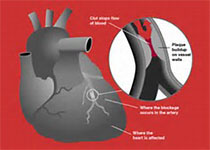
尽管一些随机对照试验(RCTs)和荟萃分析显示,延长双联抗血小板治疗(DAPT)与死亡率增加相关,但其中的作用机制仍不清楚。2017年4月,发表在《J Am Coll Cardiol.》的一项RCTs的荟萃分析调查了出血相关死亡与冠脉支架植入后DAPT治疗疗程的相关性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#冠脉支架#
42
#JACC#
40
#支架植入#
50
#ACC#
33
#DAPT#
28
#植入#
24
感谢作者分享
33
DES后不同DAPT疗程的RCT中,DAPT疗程较短,全因死亡率较低的潜在原因
46
学习了,不错
38
学习一下知识
33