Nanoscale Res Lett:使用原子力显微镜观察软骨分化人脂肪来源的干细胞
2018-11-12 MedSci MedSci原创
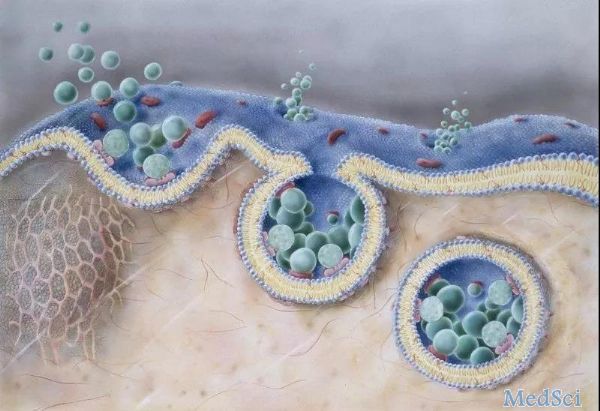
已知整联蛋白β1参与分化、迁移、增殖、伤口修复、组织发育和器官发生。为了分析整合素β1配体和分化簇29(CD29)受体之间的结合概率,使用原子力显微镜(AFM)检测人脂肪来源干细胞(hADSc)表面上的天然整合素β1偶联受体。 在二维细胞培养水平的早期软骨形成分化过程中,整合素β1-功能化尖端对hADScs探测整联蛋白β1配体-受体相互作用的结合概率。AFM测定hADSc的细胞形态和超微结构
已知整联蛋白β1参与分化、迁移、增殖、伤口修复、组织发育和器官发生。为了分析整合素β1配体和分化簇29(CD29)受体之间的结合概率,使用原子力显微镜(AFM)检测人脂肪来源干细胞(hADSc)表面上的天然整合素β1偶联受体。
在二维细胞培养水平的早期软骨形成分化过程中,整合素β1-功能化尖端对hADScs探测整联蛋白β1配体-受体相互作用的结合概率。AFM测定hADSc的细胞形态和超微结构,证明长轴细胞成为多角形细胞,长度/宽度比降低,软骨诱导过程中粗糙度增加。整合素β1配体和CD29受体的结合通过β1功能化的生存hADSc尖端检测。在软骨诱导的0、6和12天记录总共1200条曲线。平均破裂力分别为61.8±22.2 pN、60±20.2 pN和67.2±22.0 pN。破裂事件分别为19.58±1.74%、28.03±2.05%和33.4±1.89%,表明软骨诱导过程中整合素β1配体与hADSc表面受体之间的结合概率增加。整合素β1和β-连环蛋白/SOX信号通路在软骨形成分化过程中相关。
综上所述,这项研究的结果意味着AFM提供动力学和视觉洞察整合素β1配体-CD29受体在软骨形成过程中对hADSc结合的变化。细胞形态、膜超微结构和配体-跨膜受体结合概率的变化是用于评估软骨形成分化过程的有用标记物。
原始出处:
Jie Yang, Ming-Tang He, et al., Atomic Force Microscopy-Based Nanoscopy of Chondrogenically Differentiating Human Adipose-Derived Stem Cells: Nanostructure and Integrin β1 Expression. Nanoscale Res Lett. 2018; 13: 333.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#scale#
27
#骨分化#
28
#显微镜#
26