BMC Gastroenterology:内镜逆行阑尾炎治疗与腹腔镜阑尾切除术与开腹阑尾切除术治疗急性阑尾炎的疗效差异分析
2022-02-27 MedSci原创 MedSci原创
阑尾炎是因多种因素而形成的炎性改变,为外科常见病,以青年最为多见,男性多于女性。临床上急性阑尾炎较为常见,各年龄段及妊娠期妇女均可发病。
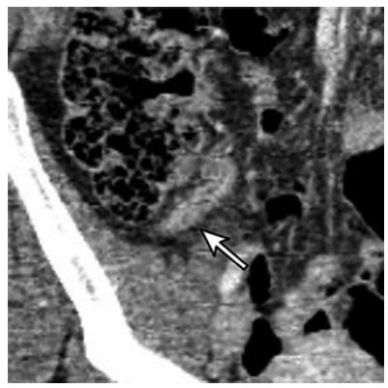
急性阑尾炎是临床上引起急性腹痛最常见的原因之一,阑尾切除术长期以来一直是急性阑尾炎的标准治疗方法。然而,存在一系列潜在的术后并发症,如术后出血、伤口感染和肠梗阻等,据报道总体并发症发生率为 8.2-31.4%。因此,开发一种安全有效的非手术方法已成为治疗急性单纯性阑尾炎的议程。受到内镜逆行胰胆管造影 (ERCP)的启发,Liu 等人首先报道了内镜下逆行阑尾炎治疗(ERAT)。ERAT 是一种治疗急性单纯性阑尾炎的新型、非手术和微创方法。本项研究旨在进行了一项前瞻性随机对照试验,比较 ERAT 与腹腔镜阑尾切除术(LA)和开腹阑尾切除术(OA),并评估 ERAT 治疗急性单纯性阑尾炎的可行性和安全性。

在这项开放标签、随机试验中,参与者被随机分配到ERAT组、腹腔镜阑尾切除术(LA)组和开放式阑尾切除术(OA)组。主要结果是治疗的临床成功率的差异。研究中使用了意向治疗分析。
该研究包括 99 名患者,每组有 33 名参与者。ERAT、LA和OA组的临床成功率分别为87.88%(29/33)、96.97%(32/33)和100%(33/33)。在 ERAT 组中,4名患者因插管困难而导致ERAT失败。LA组1例因腹腔粘连失败。三个治疗组的临床成功率无显着差异(P=0.123)。中位随访时间为 22 个月。三组不良事件发生率差异无统计学意义(P =0.693),ERAT与手术的最终成功率为21.21%(7/33)。
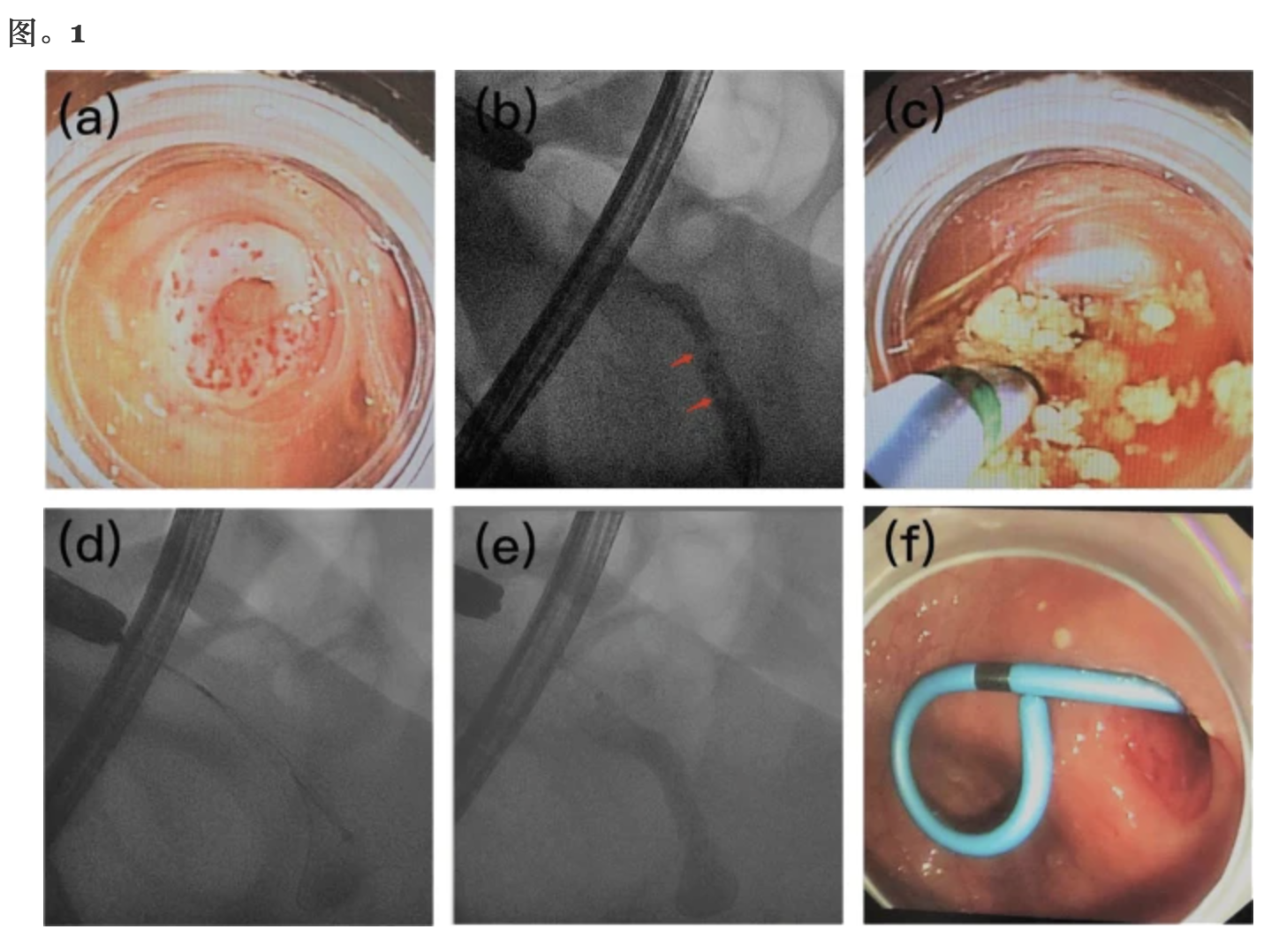
本项研究证实ERAT 治疗急性单纯性阑尾炎是可行且安全的,阑尾结石和感染被认为是导致急性阑尾炎的重要原因,ERAT 可以通过阑尾切除、脓液引流和腔内压力降低来治疗急性单纯性阑尾炎,以缓解症状,最终治疗急性阑尾炎。
原始出处:
Zhemin Shen. Et al. Endoscopic retrograde appendicitis therapy versus laparoscopic appendectomy versus open appendectomy for acute appendicitis: a pilot study. BMC Gastroenterology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#GAS#
43
#切除术#
40
#BMC#
32
#Gastroenterol#
35
#阑尾#
0
#阑尾炎#
99
#AST#
39
#内镜#
42
#腹腔镜#
50
#Gastroenterology#
38