Heart:预防外周动脉疾病 选阿托伐他汀还是辛伐他汀?
2015-01-20 小田 译 医学论坛网
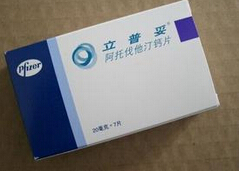
多国学者探讨了大剂量和常规剂量的他汀类药物治疗是否可减少外周动脉疾病(PAD)的发生率,以及大剂量他汀治疗对合并PAD患者的心血管疾病(CVD)转归的影响。结果显示,与常规剂量辛伐他汀相比,大剂量阿托伐他汀显著减少PAD的发生率。基线时有PAD病史的患者将来发生冠脉事件的风险较高,而大剂量阿托伐他汀治疗可减少这一风险。相关论文1月16日在线发表于《心脏》(Heart)杂志。 研究者们纳入
多国学者探讨了大剂量和常规剂量的他汀类药物治疗是否可减少外周动脉疾病(PAD)的发生率,以及大剂量他汀治疗对合并PAD患者的心血管疾病(CVD)转归的影响。结果显示,与常规剂量辛伐他汀相比,大剂量阿托伐他汀显著减少PAD的发生率。基线时有PAD病史的患者将来发生冠脉事件的风险较高,而大剂量阿托伐他汀治疗可减少这一风险。相关论文1月16日在线发表于《心脏》(Heart)杂志。
研究者们纳入了“通过积极降脂治疗进一步减少终点事件”研究中的8888例心肌梗死后患者,这些患者被随机分为大剂量或常规剂量他汀至(阿托伐他汀80 mg/d,辛伐他汀20–40 mg/d)。转归为预先设定的PAD的转归,事后分析大剂量他汀在减少PAD患者的CVD风险的效果。
结果显示,在中位随访的近5年间,在接受阿托伐他汀和辛伐他汀治疗的患者中,分别有94例(2.2%)和135例患者(3.2%)发展为PAD(HR=0.70,P=0.007)。
PAD患者的基线时严重冠脉事件风险几乎2倍高,但在校正不良心血管风险预测后这种风险不再显著。在PAD患者中,阿托伐他汀组的严重冠脉事件较少,阿托伐他汀组和辛伐他汀组分别为14.4%和20.1%,但差异未达到统计学显著性(HR=0.68,P=0.13)。同时,阿托伐他汀显著减少PAD患者的总体心血管和冠脉事件以及冠脉血运重建。
原始出处:
Stoekenbroek RM1, Boekholdt SM2, Fayyad R3, Laskey R3, Tikkanen MJ4, Pedersen TR5, Hovingh GK1; On behalf of the Incremental Decrease in End Points Through Aggressive Lipid Lowering Study Group.High-dose atorvastatin is superior to moderate-dose simvastatin in preventing peripheral arterial disease.Heart. 2015 Jan 16. pii: heartjnl-2014-306906. doi: 10.1136/heartjnl-2014-306906. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ART#
35
#辛伐他汀#
51
#HEART#
59
#外周动脉#
42