Lancet子刊:50万中国人研究提示,腔隙性脑梗并不是无害,5年复发率近40%!
2022-03-12 MedSci原创 MedSci原创
在所有无症状LACI病例中,5年内近40%的患者出现卒中复发、近10%患者死亡,这与有症状LACI的复发率及全因死亡率相近!
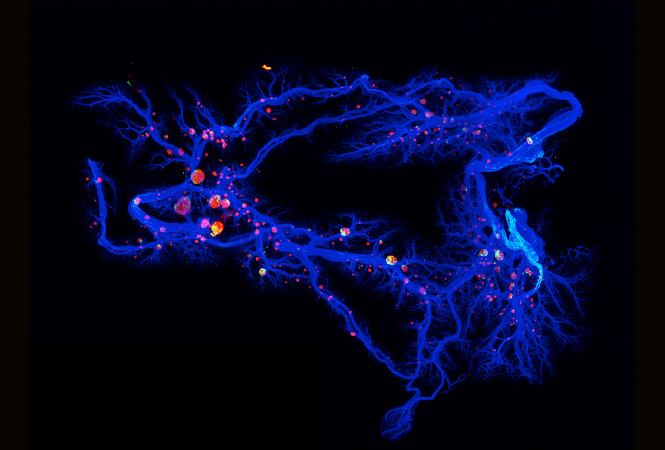
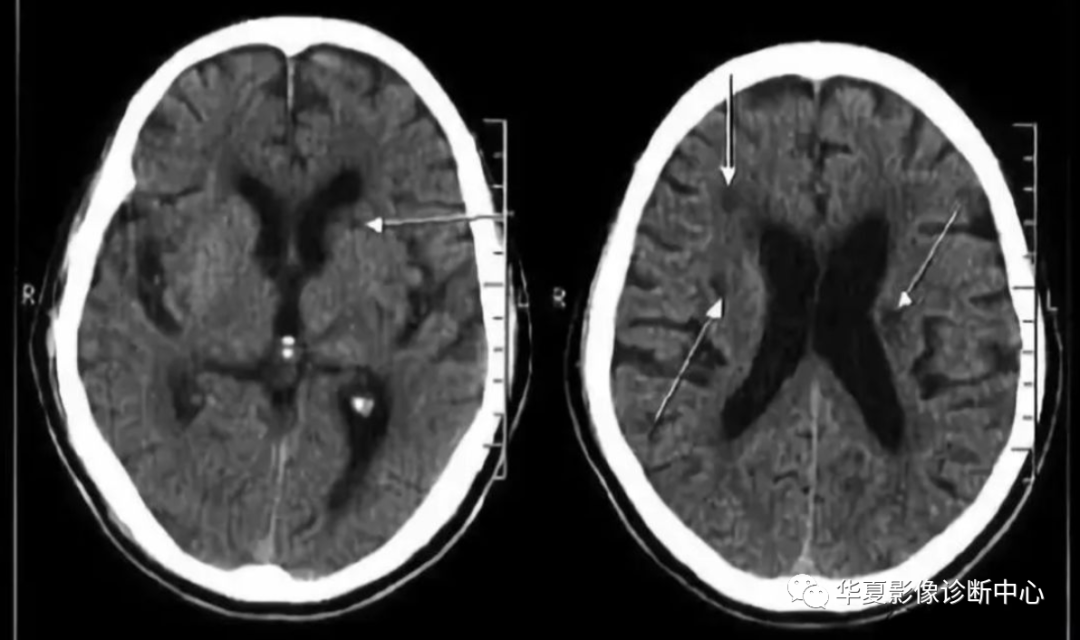
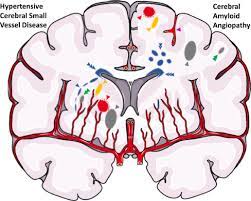
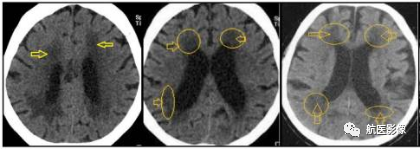
沉默的腔隙性脑梗塞(LACI)是隐蔽的脑缺血病变,通常患者出现非特异性或不典型的神经系统症状,但却没有急性卒中。LACI,或称Lacunes,是小的脑梗塞(直径<15mm),圆形或卵圆形,主要发生在大脑皮层下区域的深部小动脉区域,约占所有缺血性脑卒中(IS)的20-35%。
大约10%的LACI发现于大脑皮层区域。大多数LACI是由小动脉闭塞引起的,但大动脉粥样硬化和心脏栓塞也可能涉及。沉默的和有症状的LACI是脑小血管疾病(CSVD)谱系的一部分,包括白质增生(WMH)、血管周围空间(PVS)、脑微出血(CMB)和脑萎缩。
无症状LACI患者通常无明确的神经系统局灶性症状或体征,容易被临床忽视。为了更好的了解LACI的临床意义,近期,来自四川大学华西医院、英国牛津大学、北京天坛医院、中国医学科学院、北京大学医学部等多中心的专家开展了一项前瞻性研究,结果发表在《柳叶刀-区域健康》杂志上。
研究人员对489,597名基线时没有中风或缺血性心脏病史的中国成年人的前瞻性研究中,比较了无声腔隙梗死与有症状腔隙梗死的5年复发中风和全因死亡的风险。复发性中风和全因死亡率的数据是通过与当地中风和死亡登记处以及所有入院的健康保险记录相联系而获得的。
在12150个被裁定诊断为首次LACI的病例中,4134个(34%)为隐匿性LACI,8016个(66%)为有症状的LACI。所有病例都有脑部成像,但只有33%的隐匿性LACI和40%的症状性LACI病例有脑部磁共振成像(MRI)。
总的来说,城市地区隐匿性LACI的发生率是农村地区的2倍,但所有地区隐匿性LACI与有症状LACI的比率相似。隐匿性LACI与有症状的LACI病例的5年复发卒中风险(38% vs 43%)和全因死亡风险(11% vs 14%)分别相当。

第一次缺血性卒中事件发生后28天内复发卒中和全因死亡的累积事件率
对于隐匿性和有症状的LACI病例,大多数复发中风病例都是非LACI(70% vs 72%)。虽然复发卒中的相对风险在年龄、性别和地区上没有差异,但全因死亡率的绝对风险却因性别、年龄和地区而异。
综上,在所有无症状LACI病例中,5年内近40%的患者出现卒中复发、近10%患者死亡,这与有症状LACI的复发率及全因死亡率相近!
参考文献:
Natural history of silent lacunar infarction: 10-year follow-up of a community-based prospective study of 0.5 million Chinese adults. https://doi.org/10.1016/j.lanwpc.2021.100309
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#复发率#
50
#Lancet#
43
好文!
57
#学习#学习一下
72
#脑梗#
48