J Med Chem:新型Bcr-Abl小分子抑制剂有望用于慢粒性白血病耐药的治疗
2013-04-01 广州生物医药与健康研究院 广州生物医药与健康研究院
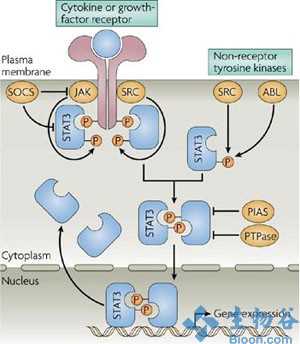
Bcr-Abl小分子抑制剂Imatinib在临床治疗慢粒性白血病(CML)等疾病方面已获得巨大成功。但由Bcr-Abl突变诱发的临床耐药已成为当今肿瘤医学的重要问题。二代药物Nilotinib和Dasatinib仅能克服部分基因突变引起的耐药,而对Bcr-AblT315I这一发生率最高的耐药突变无效。2012年12月,克服Bcr-AblT315I耐药的ponatinib才刚被美国FDA批准上市,但
Bcr-Abl小分子抑制剂Imatinib在临床治疗慢粒性白血病(CML)等疾病方面已获得巨大成功。但由Bcr-Abl突变诱发的临床耐药已成为当今肿瘤医学的重要问题。二代药物Nilotinib和Dasatinib仅能克服部分基因突变引起的耐药,而对Bcr-AblT315I这一发生率最高的耐药突变无效。2012年12月,克服Bcr-AblT315I耐药的ponatinib才刚被美国FDA批准上市,但其对Bcr-Abl E255K/V等P-Loop区突变等效果不佳。
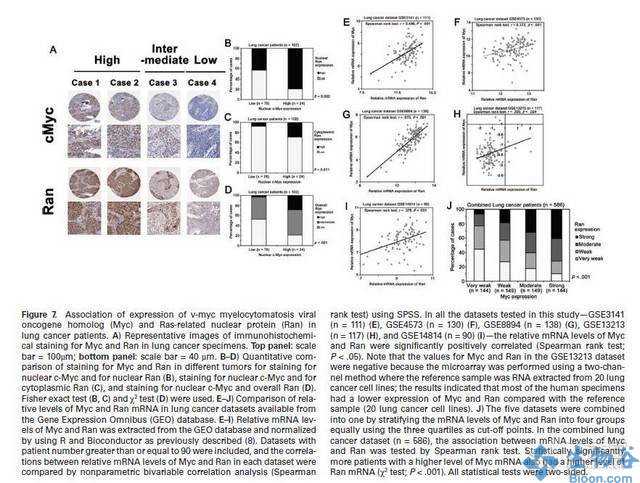
中科院广州生物医药与健康研究院丁克博士带领团队经过近4年的技术攻关,成功设计和合成了芳基炔类和三氮唑苯甲酰胺两类Bcr-Abl小分子抑制剂。化合物在多种激酶、细胞和动物模型中可有效克服Bcr-AblT315I突变诱发的耐药问题。其中,化合物GZD824可以以pM的IC50值抑制Bcr-AblWT及Bcr-AblT315I等耐药突变体的激酶活性(分别为0.34和0.68 nM),并对P-loop区突变(E255K/V)等有效。化合物在多种细胞和动物模型中表现出优异抗肿瘤活性(针对K562,Ku812等CML肿瘤细胞的IC50为0.2~10 nM;针对携带Bcr-AblT315I 突变体的Ba/F3细胞的IC50约为7 nM;在1.0-20.0 mg/kg/day 的口服剂量下完全抑制肿瘤生长)和较好的安全性指标及优异的药代动力学性质(大鼠口服生物利用度约为48.7%;体内半衰期T1/2约为8-10小时)。目前,GZD824已被确定为候选药物,正在进行规范的临床前评价。以该项目为基础,研究团队还获得2011年“第四届中国科学院青年创业大赛”金奖。
该项研究获得国家新药创制重大专项、广东省新药创制重大专项、广州市重大专项以及中科院交叉团队项目等资助。部分结果已在药物化学期刊J. Med. Chem. 发表。

doi:10.1021/jm301581y
PMC:
PMID:
Xiaomei Ren †‡, Xiaofen Pan †, Zhang Zhang †, Deping Wang †§, Xiaoyun Lu †, Yupeng Li †§, Donghai Wen †, Huoyou Long †, Jinfeng Luo †, Yubing Feng †, Xiaoxi Zhuang †, Fengxiang Zhang †, Jianqi Liu †, Fang Leng †, Xingfen Lang †, Yang Bai †, Miaoqin She †, Zhengchao Tu †, Jingxuan Pan ‡, and Ke Ding *†
Bcr-AblT315I mutation-induced imatinib resistance remains a major challenge for clinical management of chronic myelogenous leukemia (CML). Herein, we report GZD824 (10a) as a novel orally bioavailable inhibitor against a broad spectrum of Bcr-Abl mutants including T315I. It tightly bound to Bcr-AblWT and Bcr-AblT315I with Kd values of 0.32 and 0.71 nM, respectively, and strongly inhibited the kinase functions with nanomolar IC50 values. The compound potently suppressed proliferation of Bcr-Abl-positive K562 and Ku812 human CML cells with IC50 values of 0.2 and 0.13 nM, respectively. It also displayed good oral bioavailability (48.7%), a reasonable half-life (10.6 h), and promising in vivo antitumor efficacy. It induced tumor regression in mouse xenograft tumor models driven by Bcr-AblWT or the mutants and significantly improved the survival of mice bearing an allograft leukemia model with Ba/F3 cells harboring Bcr-AblT315I. GZD824 represents a promising lead candidate for development of Bcr-Abl inhibitors to overcome acquired imatinib resistance.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
37
#小分子#
36
#小分子抑制剂#
55
#Med#
0