Cardiovasc Diabetol:在2型糖尿病中,AGEs和可溶性RAGE亚型的循环水平与全因死亡率和心血管并发症的发生有关
2022-07-10 从医路漫漫 MedSci原创
AGEs是蛋白质和脂质的非酶糖基化和氧化的产物,在生理条件下,抗糖基化防御足以防止其积累。
背景:晚期糖基化终产物(AGEs)和晚期糖基化终产物受体(RAGE)激活细胞信号通路,调节几种慢性炎症疾病的炎症基因表达谱。AGEs是蛋白质和脂质的非酶糖基化和氧化的产物,在生理条件下,抗糖基化防御足以防止其积累。在衰老和年龄相关疾病(ARDs)中,主要是在糖尿病中,AGEs的负担显著增加,使用皮肤自体荧光测量的AGEs水平与多种慢性疾病中主要心血管不良事件(MACE)的发生率显著增加相关,包括心力衰竭、二型糖尿病和终末期肾病。AGEs在促进内皮功能障碍和加重动脉粥样硬化中的作用已被证实,它们与动脉僵硬度的非侵入性测量密切相关,这在男性和年轻个体中更明显。膜结合RAGE (FL-RAGE)是一种识别AGEs和其他几种配体的模式识别受体,其中一些作为损伤相关分子模式(DAMPS)和病原体相关分子模式(PAMPs)。在生理条件下,RAGE在肺中表达,而在其他组织中几乎检测不到;然而,其水平是由配体积累诱导的。
RAGE的可溶形式,统称为(sRAGE),也存在于血液中,由RAGE胞外域组成,通过金属蛋白酶对膜结合形式的蛋白水解切割(cRAGE)或通过选择性剪接产生,作为内源性分泌RAGE (esRAGE),其被积极分泌。sRAGE在配体结合时不转导信号,充当诱饵分子来抑制RAGE/配体诱导的细胞活化。因此,服用sRAGE可减少糖尿病和动脉粥样硬化组织重塑、年龄相关的心脏纤维化和血管损伤后的新内膜扩张。在人类中,循环sRAGE和esRAGE水平的改变与疾病状态或其风险因素有关。许多研究报告称,患有代谢综合征、高血压、肥胖症和糖尿病前期等心脏代谢疾病的受试者的sRAGE或esRAGE水平较低。健康受试者的sRAGE也会随着年龄的增长而降低。相比之下,年龄升高与慢性糖尿病肾功能减退的人有关。sRAGE作为疾病和不良事件发生标志的潜在预后价值似乎适用于患有慢性疾病或多病的个体,而不适用于普通人群。关于糖尿病,sRAGE浓度增加与1型糖尿病的全因死亡率和心血管(CV)死亡率增加相关。在二型糖尿病患者中,较高水平的sRAGE与5年以上随访中新发或恶化的肾脏疾病和死亡率独立相关。前瞻性研究强调,在2型糖尿病,sRAGE和esRAGE与冠心病(CHD)事件之间存在显著的正相关。
最近,AGEs/sRAGE的比值被认为是比单独的AGEs或sRAGE变异体更有效的器官损伤生物标志物。此外,最近证实了作为心血管危险因素标志的esRAGE和cRAGE的不同预测能力。例如,我们已经发表了在健康人群和长寿个体(LLIs)中,cRAGE与衰老负相关,而esRAGE是肥胖和长寿的更合适的生物标志物。因此,为了确定AGEs/sRAGE亚型轴在人类病理学中的预后价值,应该考虑新的方面。RAGE的胞质结构域与formin膜1结合,formin膜1对于RAGE/配体介导的活性氧簇(ROS)的活化和产生至关重要,最终促进ARDs的炎症过程。
目的:我们同时测定了二型糖尿病患者和年龄、性别匹配的健康对照受试者中两种sRAGE亚型——esRAGE和cRAGE——AGEs的循环水平及其各自的比率,并研究了它们与2型糖尿病15年全因死亡率的关系。
方法:用ELISA法测定362例二型糖尿病患者和125例年龄和性别匹配的健康对照者(CTR)的基线年龄和sRAGE亚型浓度。使用Cox比例风险模型确定死亡率的独立预测因子,并用于建立和验证二型糖尿病全因死亡率预测的列线图。
结果:与对照组相比,二型糖尿病病患者的年龄、总年龄、cRAGE、年龄/年龄和年龄/年龄比值显著增加(p < 0.001)。在CTR受试者中,而不是在二型糖尿病患者中,cRAGE和年龄之间的显著负相关被证实(p = 0.003),而AGEs/sRAGE (p = 0.032)和AGEs/cRAGE (p = 0.006)比值与年龄正相关。平均随访15年(4,982人年),观察到130例死亡。在二型糖尿病患者中,年龄/年龄比值的增加伴随着更高的全因死亡率风险(HR每标准差增量= 1.30,95% CI 1.15–1.47;p < 0.001)。此外,在既往无主要不良心血管事件(MACE)的二型糖尿病患者中,sRAGE与主要不良心血管事件(MACE)的发生相关(或标准差每增加1.48,95% CI 1.11–1.89)。基于年龄、性别、HbA1c、收缩压和年龄/年龄比的列线图被用来预测二型糖尿病的5年、10年和15年生存率。将患者分为monogram评分的四分位数,Kaplan-Meier生存曲线证实了该模型的预后准确性(log-rank p = 6.5×1013)。
表1健康对照者(CTR)和2型糖尿病病患者年龄、sRAGE亚型及其比值的比较

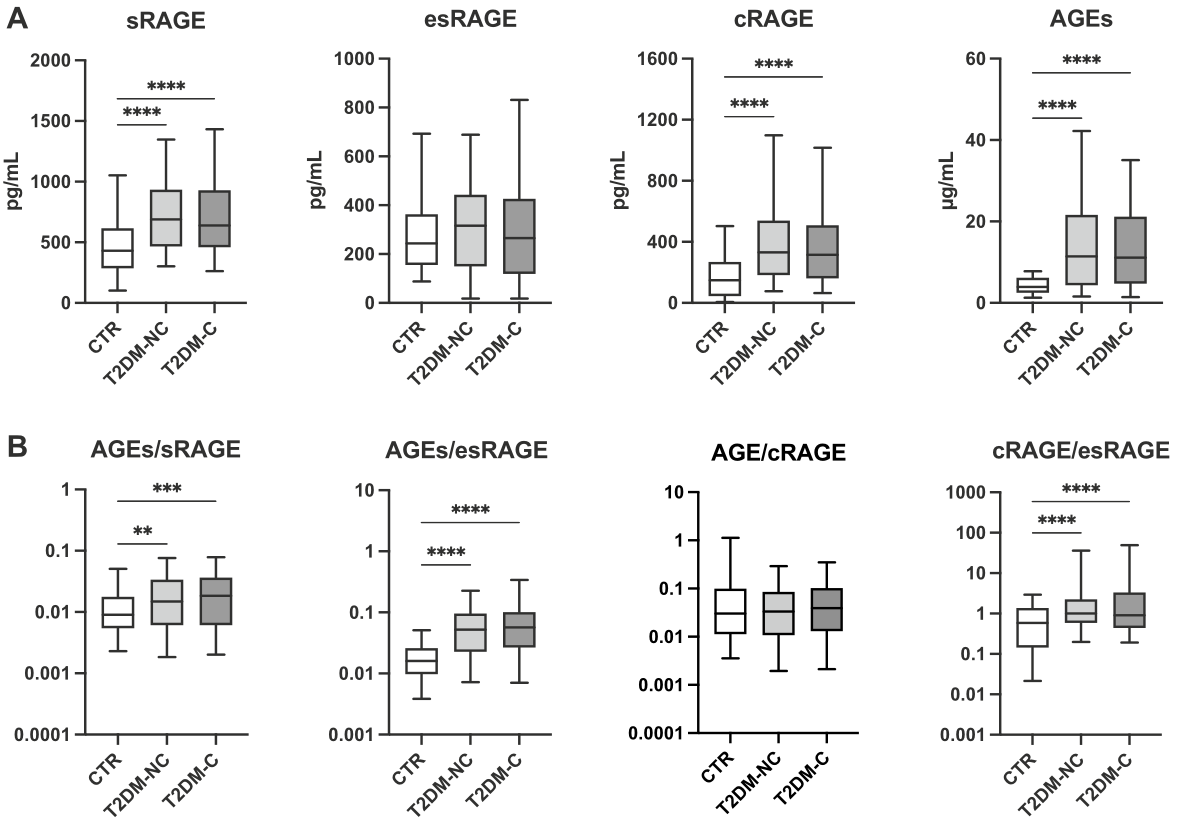
图1比较健康对照受试者(CTR)和无(T2DM-NC)或有(T2DM-C)并发症的二型糖尿病患者之间的总年龄、esRAGE和cRAGE亚型以及年龄/年龄、年龄/esRAGE、年龄/cRAGE、cRAGE/ esRAGE比率的箱线图。* * p < 0.01* * * p < 0.001* * * * Kruskal-Wallis H试验后的邓恩事后试验p < 0.0001
表2健康对照(CTR)和二型糖尿病病患者年龄和不同亚型的Spearman相关性

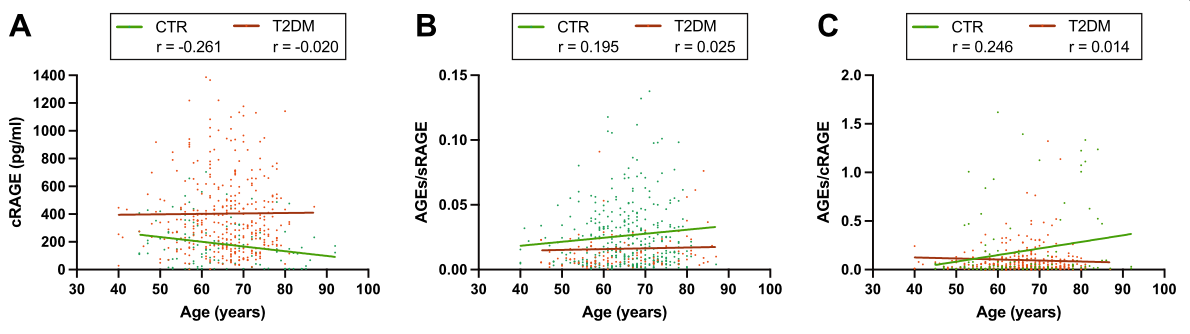
图2散点图显示受试者年龄与循环A、B年龄/年龄和C年龄/年龄比值的相关性。显示CTR(绿色)和二型糖尿病(T2DM,红色)患者的回归线

图3相关图显示了不同变量和年龄、sRAGE亚型之间的相关性以及分别在整个人群和CTR和二型糖尿病(T2DM)受试者中的衍生比率。颜色的强度取决于Spearman相关的大小。非显著相关(p ≥ 0.05)交叉
结论:年龄和cRAGE亚型的比值可以预测2型糖尿病患者的15年生存率。我们的数据支持将2型糖尿病患者的循环AGE和可溶性RAGE亚型作为MACE和全因死亡率的预测因子。
原文出处:Sabbatinelli J, Castiglione S, Macrì F,et al.Circulating levels of AGEs and soluble RAGE isoforms are associated with all-cause mortality and development of cardiovascular complications in type 2 diabetes: a retrospective cohort study.Cardiovasc Diabetol 2022 Jun 06;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#并发#
56
#BET#
40
#GES#
48
#ASC#
37
#DIA#
44
#全因死亡率#
68
#AGEs#
42
#心血管并发症#
43
#血管并发症#
34