骨质疏松8大误区 10个问题自我检测
2015-10-20 王宇鹏 北京市疾控中心
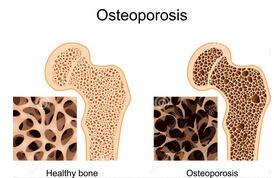
许多人到了中老年的时候个子会变“矮”,这其实是人体骨骼逐渐衰退的表现,最主要的“元凶”就是骨质疏松。作为中老年人最常见的骨骼疾病,由骨质疏松引起的骨折,轻则影响机体功能,重则致残甚至致死。10月20日是世界骨质疏松日,我们在认识和防治骨质疏松方面,存在哪些误区?有哪些办法可以自测是否为高危人群? 骨质疏松常见的8大误区: 1.喝骨头汤能防止骨质疏松 实验证明,同样一碗牛奶中的钙含量要远远高于
许多人到了中老年的时候个子会变“矮”,这其实是人体骨骼逐渐衰退的表现,最主要的“元凶”就是骨质疏松。作为中老年人最常见的骨骼疾病,由骨质疏松引起的骨折,轻则影响机体功能,重则致残甚至致死。10月20日是世界骨质疏松日,我们在认识和防治骨质疏松方面,存在哪些误区?有哪些办法可以自测是否为高危人群?
骨质疏松常见的8大误区:
1.喝骨头汤能防止骨质疏松
实验证明,同样一碗牛奶中的钙含量要远远高于一碗骨头汤。对老人而言,骨头汤里溶解了大量骨内脂肪,经常食用还可能引起其他健康问题。
2.治疗骨质疏松症等于补钙
简单来讲骨质疏松症是骨代谢的异常(人体内破骨细胞影响大于成骨细胞,以及骨吸收的速度超过骨形成速度)造成的。因此骨质疏松症的治疗不是单纯补钙,而是综合治疗,提高骨量、增强骨强度和预防骨折。患者应当到正规医院进行诊断和治疗。
3.骨质疏松症是老年人才有的现象
骨质疏松症并非是老年人的“专利”,如果年轻时期忽视运动,常常挑食或节食,饮食结构不均衡,导致饮食中钙的摄入少,体瘦,又不拒绝不良嗜好,这样达不到理想的骨骼峰值量和质量,就会使骨质疏松症有机会侵犯年轻人,尤其是年轻的女性。
4.老年人治疗骨质疏松症为时已晚
很多老年人认为骨质疏松症无法逆转,到老年期治疗已没有效果,为此放弃治疗,这是十分可惜的。从治疗的角度而言,治疗越早,效果越好。所以,老年人一旦确诊为骨质疏松症,应当接受正规治疗,减轻痛苦,提高生活质量。
5.靠自我感觉发现骨质疏松症
多数骨质疏松症病人在初期都不出现异常感觉或感觉不明显。发现骨质疏松症不能靠自我感觉,不要等到发觉自己腰背痛或骨折时再去诊治。高危人群无论有无症状,应当定期去具备双能X线吸收仪的医院进行骨密度检查,有助于了解您的骨密度变化。
6.骨质疏松症是小病,治疗无须小题大做
骨质疏松症平时不只是腰酸腿痛而已,一旦发生脆性骨折,尤其老年患者的髋部骨折,导致长期卧床,死亡率甚高。
7.骨质疏松容易发生骨折,宜静不宜动
保持正常的骨密度和骨强度需要不断地运动刺激,缺乏运动就会造成骨量丢失。体育锻炼对于防止骨质疏松具有积极作用。另外,如果不注意锻炼身体,出现骨质疏松,肌力也会减退,对骨骼的刺激进一步减少。这样,不仅会加快骨质疏松的发展,还会影响关节的灵活性,容易跌倒,造成骨折。
8.骨折手术后,骨骼就正常了
发生骨折,往往意味着骨质疏松症已经十分严重。骨折手术只是针对局部病变的治疗方式,而全身骨骼发生骨折的风险并未得到改变。因此,我们不但要积极治疗骨折,还需要客观评价自己的骨骼健康程度,以便及时诊断和治疗骨质疏松症,防止再次发生骨折。
骨质疏松症高危人群的自我检测:
以下问题可以帮助进行骨质疏松症高危情况的自我检测,任何一项回答为“是”者,则为高危人群,应当到骨质疏松专科门诊就诊:
1.您是否曾经因为轻微的碰撞或者跌倒就会伤到自己的骨骼?
2.您连续3个月以上服用激素类药品吗?
3.您的身高是否比年轻时降低了三厘米?
4.您经常过度饮酒吗?(每天饮酒2次,或一周中只有1-2天不饮酒)
5.您每天吸烟超过20支吗?
6.您经常腹泻吗?(由于腹腔疾病或者肠炎而引起)
7.父母有没有轻微碰撞或跌倒就会发生髋部骨折的情况?
8.女士回答:您是否在45岁之前就绝经了?
9.您是否曾经有过连续12个月以上没有月经(除了怀孕期间)?
10.男士回答:您是否患有阳痿或者缺乏性欲这些症状?
(王宇鹏综合自北京市疾控中心网站)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













正确的运动是健康之本
75
不错,赞一个
118
关键得锻炼
122
学习了…
107
好东西
119
有用、很好!
73
要服用双膦酸盐抑制破骨细胞活性
94
#误区#
29
#骨质#
35
锻炼为主
71