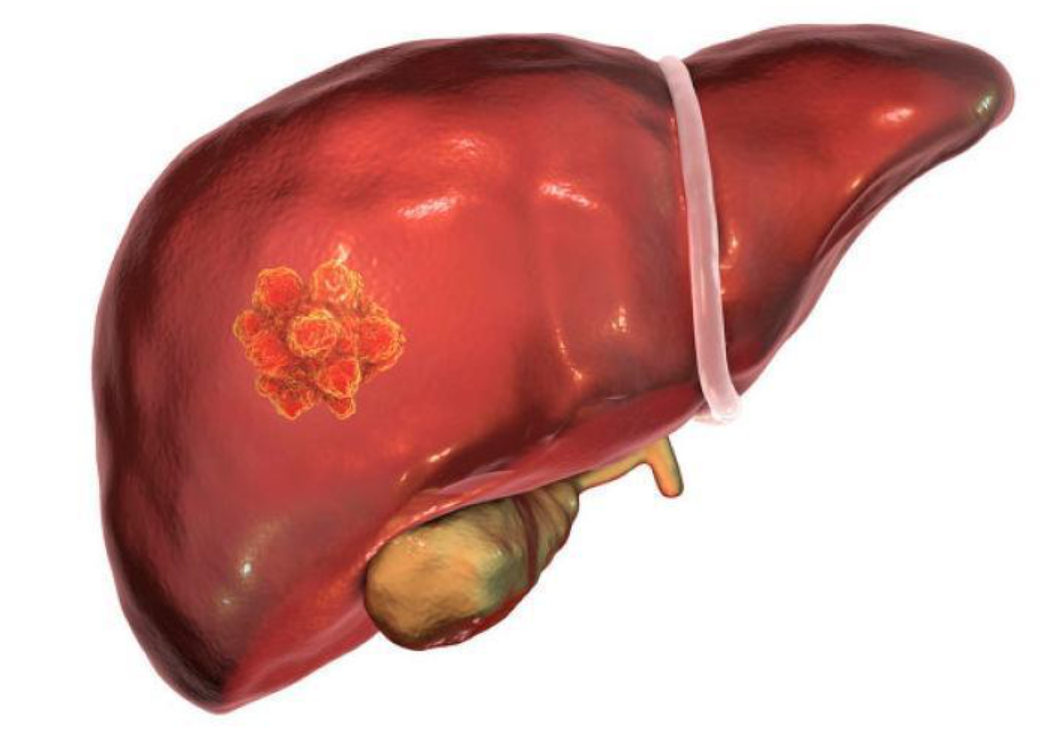
Liver Cancer:新开发的改良ALBI分级显示更好的肝细胞癌预后和预测价值
2021-12-11 yd2015 MedSci原创
研究表明,新开发的改良ALBI(mALBI)分级标准是肝细胞癌患者更好的预后和预测指标,值得临床推广。
传统上,Child Pugh分级被用作评估肝细胞癌(HCC)患者肝功能储备的指标。然而,它也有一些缺点。它的五个组成因素中的两个,肝性脑病和腹水,是主观的,血清白蛋白水平和腹水是混杂因素。此外,不同等级患者的分布严重倾斜,Child Pugh A患者约占所有患者的三分之二。2015年,Johnson等人提出白蛋白-胆红素分级(ALBI)作为一种新的方法。评分分为1 - 3级:≤-2.60(1级),>-2.60和≤-1.39(2级), >-1.39(3级),1级表示肝损害最小。目前有多个研究表明,ALBI分级能够比Child Pugh分级提供更详细的预后分类。而目前也有提出ALBI分级出现一些缺点,因为按标准各分级的人员严重的倾向。因此,来自日本的Masatoshi Kudo教授开展相关研究,发现新开发的改良ALBI(mALBI)分级标准是肝细胞癌患者更好的预后和预测指标,相关研究结果发表在Liver Cancer杂志上。

新开发的改良ALBI分级标准是2017年Hiraoka教授提出,将ALBI 2级患者进一步分为2a和2b级,这样可进一步平衡各组的人员。
本研究将85,636例HCC患者根据Child Pugh分级和改良ALBI(mALBI)分级进行预后分析。研究表明,所有HCC患者,改良ALBI分级能够更好的鉴定出预后好的患者。Child Pugh A患者的中位总生存期(OS)为80个月,而mALBI 1级患者的中位总生存期为103个月。

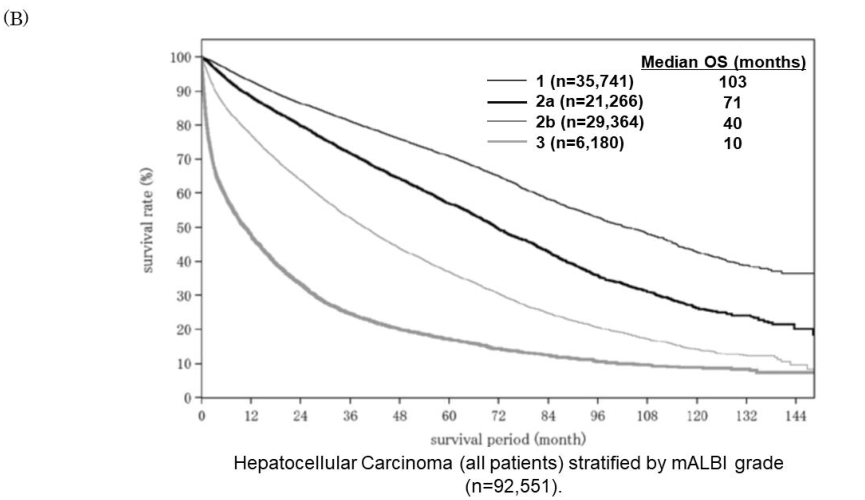
所有患者两种分级标准预后对比
另外,对于手术切除的HCC患者,改良ALBI分级能够更好的鉴定出预后好的患者。mALBI 1级和Child Pugh A患者的中位OS分别为123个月和105个月。而mALBI 3级和Child Pugh C患者的中位OS分别为45个月和23个月。
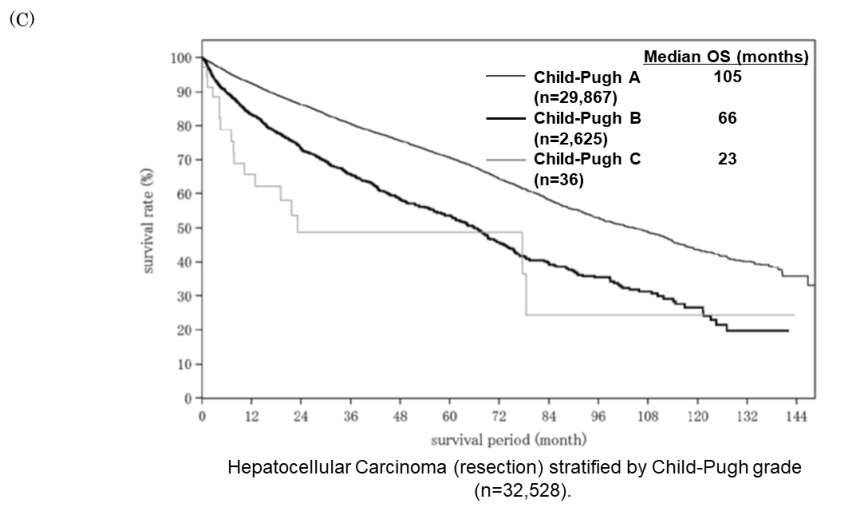
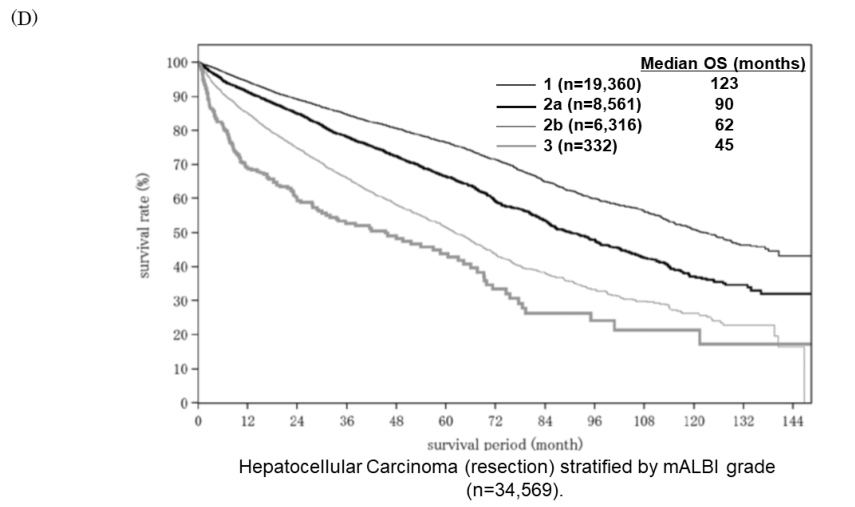
手术患者两种分级标准预后对比
对于消融治疗的HCC患者,mALBI 1级患者的中位OS优于Child Pugh A患者(分别为110个月vs. 87个月),mALBI 3级患者的中位OS优于Child Pugh C患者(分别为35个月vs. 28个月)。mALBI 2a和mALBI 2b患者数量分布非常均匀,切除组和消融组mALBI分级分层性能均较好。
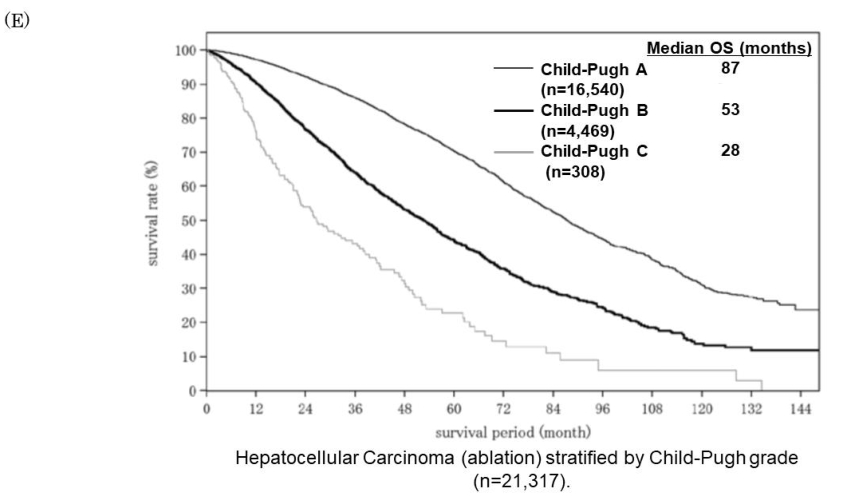

消融治疗患者两种分级标准预后对比
对于TACE治疗HCC患者,mALBI 1级患者的中位OS为61个月,优于Child Pugh A患者的47个月。在接受其他治疗的患者中观察到,mALBI 3级患者的中位OS为18个月,也优于Child Pugh C患者的14个月。
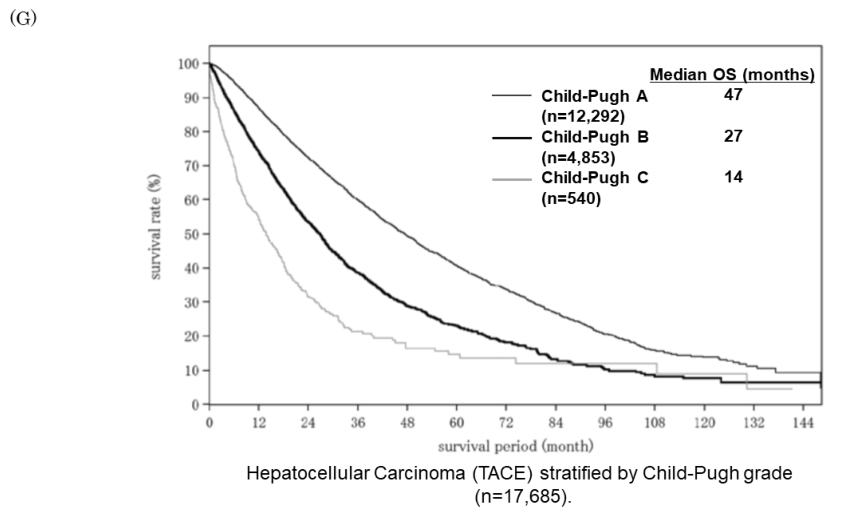

TACE治疗患者两种分级标准预后对比
对于系统性化疗HCC患者,mALBI 1级患者12个月和15个月的中位OS优于Child Pugh A级患者,这表明mALBI分级是一个非常有用的预后因素。此外,在接受全身治疗的患者中,mALBI 2a级患者的中位OS为11个月,而mALBI 2b级患者的中位OS为7个月,这清楚地表明,即使在ALBI 2级患者中,也存在预后明显不同的亚组。研究表明,接受全身治疗且较差mALBI评分 (2b或3)的患者对分子靶向药物的反应不佳,因为他们更容易发生不良事件和计量调整。因此,使用mALBI分级来识别哪些患者属于mALBI 2b亚组是非常重要的。

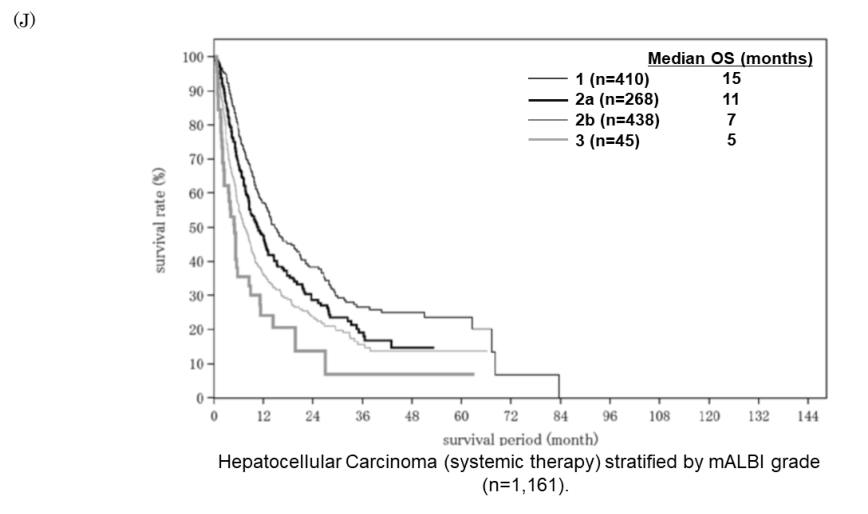
系统性化疗患者两种分级标准预后对比
综上,研究表明,新开发的改良ALBI(mALBI)分级标准是肝细胞癌患者更好的预后和预测指标,值得临床推广。
原始出处:
Masatoshi Kudo. Newly Developed Modified ALBI Grade Shows Better Prognostic and Predictive Value for Hepatocellular Carcinoma. Liver Cancer , DOI: 10.1159/000521374. Published online: December 8, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#细胞癌#
46
#肝细胞#
37
#ALBI#
48
学习新知识
67
#预测价值#
47