头痛医头,脚痛医脚,胃痛医胃?检验带给你不一样的答案
2022-02-19 刘灿华、李冉 广东省第二中医院 “检验医学”公众号
诸多疾病的临床表现并非如照教科书上描述般典型,同样的疾病在不同的患者之间表现也具有差异性。
前 言
诸多疾病的临床表现并非如照教科书上描述般典型,同样的疾病在不同的患者之间表现也具有差异性。一般排查及考虑疾病方向的原则是先易后难先常见后少见,但有时临床症状表现不那么明显以及有其他干扰症状时,会给临床诊断与鉴别诊断带来一定的困惑,这就需要临床医生具备更丰富的经验、更宽阔的思维来尽快找到真正一元论的源头。而在此过程中,我们检验项目是否也能发挥相应的作用,尽早协助临床明确诊断,找出元凶呢?有时一个简单的血常规检查就可以做到这一点。
血常规是临床上最基础的检验项目之一,其意义在于可以发现许多全身性疾病的早期迹象,协助诊断是否存在感染、贫血,初步了解是否有血液系统疾病、反应骨髓造血功能等作用。
案例经过
患者,女性,60岁,上腹部隐痛半年余,加重10余天,恶寒发热,乏力,纳差,呕吐,辗转就诊于外院,先后诊断为“慢性胃炎、肺炎、功能性胃肠病”,并予以抗感染、护胃等对症治疗后,效果不佳,遂转至我院,我院以“慢性胃炎”收入脾胃科。
外院(两家汇总)检查结果:1.查胃镜示:慢性浅表性胃炎(糜烂型)2.肠镜示:大肠多发性息肉,慢性大肠炎3.胸部CT示:左肺下叶少许炎症,双肺上叶少许纤维化、增殖灶,并临近胸膜粘连增厚4.B超示:肝胆胰脾、双肾、膀胱、子宫未见明显异常。
患者收入我院后次日完善血常规检测,结果如下图:
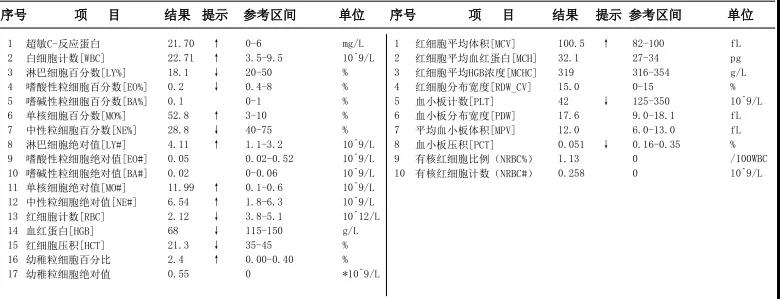
结果显示:贫血,血小板减少,白细胞升高伴单核细胞比例明显增高,其中单核细胞比例及绝对值升高,血小板减少以及血红蛋白降低均触犯了我科的复检规则(单核细胞首次绝对值>1.5×109/L,血小板首次计数小于80×109/L,血红蛋白首次检测低于70g/L)。
首先检查标本状态确实较稀,符合贫血的状态,再查看仪器报警信息:原始细胞?异常淋巴细胞?未成熟粒细胞?有核红细胞,单核细胞增多,淋巴细胞增多,白细胞增多,贫血,血小板减少。
人工推片镜检,镜下血小板无聚集,数量与仪器结果相符,可见单核细胞明显增多且多为成熟型,同时可见少量原始细胞(2%)及原幼样细胞,原幼样细胞呈单核样,个别细胞细胞胞浆中可见Auer小体(红色箭头所指),显微镜下形态如下。

至此,元凶指向性已经很明确了,血液病。立即备注报告,联系临床说明情况。由于我院未开展血液科,不具备化学染色等实验条件,建议患者到其他医院血液专科就诊,进一步完善骨髓穿刺,免疫分型以及分子遗传学等检查以明确诊断。很快,患者外院确诊为慢性粒-单核细胞白血病。
案例分析
白血病患者常见临床表现为头晕乏力、发热、感染、出血、骨痛,伴或不伴肝脾淋巴结肿大,表现在外周血常表现为:贫血、血小板减少、白细胞升高、正常或减低,且因仪器检测特性,外周血存在原始或异常细胞时,或者不分类,或者被划分为单核或淋巴细胞,导致其比例升高。所以在遇到上述情况时,就需要全面分析,警惕血液病的可能,而镜检则是必不可少的有效方法。
该患者血常规显示贫血、血小板减少,单核细胞比例及绝对值明显升高,仪器报警提示:原始细胞,这就值得我们警惕了,虽然患者的临床表现主要为胃肠道症状,但千万不能局限思维,仅仅往胃炎方向考虑,虽然长期胃炎也可导致营养不良性贫血,但单核细胞比例如此之高,贫血、血小板减少都触犯镜检规则的情况下,还是不能只是想当然,需要详细分析引起贫血及血小板减少的原因,综合分析,需要按照复检规则进行基本的推片染色镜检,观察细胞形态,并查找有无异常细胞。尽快为患者的诊断找到正确的方向。
Auer小体是在外周血或骨髓涂片白细胞胞质中出现染红色细杆状物质,1条或数条不等,长1~6um,其对白血病的诊断以及白血病细胞类型的鉴别有一定的参考价值,Auer小体主要出现于急性粒细胞和单核细胞白血病之中,是区分髓系与淋系血液肿瘤的重要形态学标志,也可见于骨髓增生异常综合征MDS-REAB-II,或者MDS/MPN(CMML)之中。而该患者血涂片可见原始细胞,且部分细胞胞浆可见Auer小体,再加上血象变化,明确指向髓系血液病。但患者外周血原始细胞比例未达20%,单凭外周血象难以明确是急性白血病还是其他,尚需结合骨穿等结果进一步明确诊断。
文献回顾
慢性粒-单核细胞白血病(CMML)是最常见的骨髓增生异常/骨髓增殖性肿瘤(MDS/MPN),年发病率为(3~4)/10万[1],其中位诊断年龄为65-70岁,年轻人很少见。由于CMML总的发病率较低、临床特征有很大的异质性且对其认识不足,因此关于其诊断和治疗进展较缓慢。
WHO2016年版骨髓增生异常/骨髓增殖性肿瘤(MDS/MPN)分类包括[2]:
1、CMML
2、aCML,BCR/ABL-(不典型慢性髓系白血病)
3、JMML(幼年型粒单核细胞白血病)
4、MDS/MPN-RS-T(骨髓增生异常/骨髓增殖性肿瘤伴环形铁粒幼细胞和血小板增多)
5、MDS/MPN-U(骨髓增生异常/骨髓增殖性肿瘤,不能分类)
CMML是一种外周血MO#>1.0×109/L,MO%≥10%,可伴形态学发育异常,骨髓及外周血原始细胞<20%的疾病,有潜在向急性白血病转化的风险。
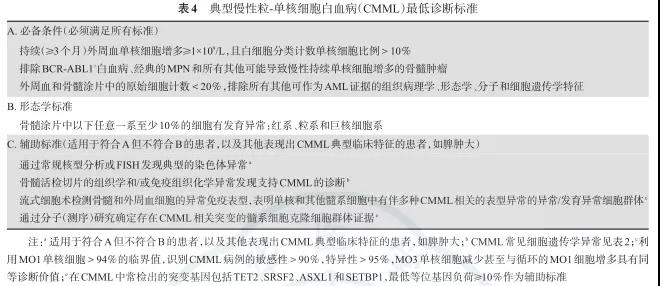
WHO给出的CMML的诊断标准为[2]:
A、外周血单核细胞持续增多(>1.0×109/L),单核细胞≥WBC计数10%。
B、不符合WHOBCR-ABL阳性CML、PMF、PV、ET诊断标准。
C、PDGFRα、PDGFRβ、FGFR1重排阴性,PCM1-JAK2突变阴性(尤其是伴有嗜酸性细胞增多时),骨髓及外周血(髓系)原始细胞<20%,一系或多系(髓系)病态造血。
D、如果未见病态造血或者病态造血少见,则需满足以下条件可诊断:
1.存在获得性克隆细胞或分子遗传学异常
2.单核细胞增多持续至少3个月
3.排除其他单核细胞增多的原因(如感染、炎症和肿瘤)
其最低诊断标准如下表1,根据WHO(2016)分型标准:依据外周血和骨髓原始细胞比例进一步分为以下3型:①原始细胞外周血中<2%和(或)骨髓中<5%者,诊断为CMML-0;②原始细胞外周血中2%~4%和(或)骨髓中5%~9%者,诊断为CMML-1;③原始细胞外周血中5%~19%,骨髓中10%~19%,和(或)有Auer小体,诊断为CMML-2。
表1典型慢粒单核细胞白血病(CMML)最低诊断标准
其与其它疾病的鉴别诊断:1)反应性单核细胞增多症:亚急性细菌性心内膜炎、结核病、疟疾感染、EB病毒感染、梅毒、伤寒、慢性和急性自身免疫性疾病等,应仔细询问病史,必要时进行相关实验室检查以除外这些可导致反应性单核细胞增多的可能原因和疾病。
(2)伴单核细胞增多的克隆性血液系统疾病:可伴单核细胞增多的克隆性血液系统疾病包括MDS伴单核细胞增多、单核细胞AML、MPN伴单核细胞增多、GATA2缺陷伴单核细胞增多、幼年型粒单细胞白血病(JMML)和组织细胞增多症等
CMML患者总体预后差,一些新药的应用可能使患者的生存期延长,改善生存质量。对于一小部分采用新药治疗达到完全缓解的患者,异基因造血干细胞移植有可能使疾病得到治愈。
总 结
该案例患者外周血可见原始及原幼样细胞,但总体比例不足20%,外周血可见Auer小体,外院行进一步检查后确诊为CMML,具体检测数据难以获得,但根据上述文献回顾内容结合其最终诊断可以推断:该患者骨髓涂片中原始细胞比例应<20%,且已进行相应基因检测,排除WHO中重现性染色体异常的AML,排除WHOBCR-ABL阳性CML、PMF、PV、ET诊断标准,排除其他单核细胞增多的原因,且因该患者血片查见Auer小体,最终诊断应为CMML-2。
该患者在外院针对“肺炎”“功能性肠胃病”对症处理后治疗效果不佳,究竟为何呢?是治疗不当还是没有找到真正的元凶?血液病其中一个临床表现就是感染,而临床常见的感染部位多为呼吸道感染、皮肤粘膜感染及胃肠道感染,而该患者同时也有白血病其他的临床症状,如贫血(乏力)、出血等。
那么当时患者在外院就诊时有没有相应进行相应的检验检查,有没有发现其异常?结果均不得而知,所幸该患者在转入我院后第一次血常规检测即发现了端倪,及时明确诊断,有效进行治疗。也再次提示我们,不可忽视血常规复检的作用。
作为检验人员,在血常规检查过程中,我们要严格遵循本科室制定的镜检规则,时刻关注仪器的报警信息,严格按照规定进行操作,不可抱有侥幸心理,若患者检测结果触犯镜检规则且确实存在异常情况,而我们并未涂片镜检,极易导致临床出现误诊及漏诊,进而对临床诊断准确性造成影响,降低临床治疗效果。
而这例病例就是通过检验人员及时推片镜检协助临床尽早明确诊断方向,避免了“胃痛医胃”,缩短了诊断时间。所以,我们不但应重视血常规复检的应用,保证血常规检验的质量,也应意识到检验在临床诊疗中的价值。
专家点评
谭俊青 广东省第二中医院检验科主任/主任技师
实验室所掌握的患者样本信息很多时候并不能全权反馈给临床医生,否则会干扰临床医生视听,而我们就要做好这个排头兵和第一道过滤作用,准确提取样本背后的有效信息反馈给临床,而非只是单纯一堆数字报告。虽然我们与患者联系不如临床那么紧密,但也不可忽视自身在患者诊疗过程中的价值。随着体外诊断在临床诊疗过程中的作用日渐加强,我们检验人员更应在加强责任心的同时不断修炼自身技能。单从血常规审核方面来讲,一方面要提高自身对异常细胞的辨识能力,另一方面需要掌握各类血液病的临床表现及实验室检查结果特点,才能做到慧眼识异,真正发挥检验在临床诊疗工作中的价值。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#胃痛#
41
学习了,谢谢分享
58
学习一下
55
学习
51
学习
54
学习
48
非常好,感谢推荐
19
学习
18