Nat Commun:EZH2甲基化ERG K362位点并增强前列腺癌中TMPRSS2-ERG的致癌活性
2021-07-14 xiaozeng MedSci原创
ETS转录因子是一类控制细胞增殖、分化和致癌作用的信号依赖性转录调节因子家族。
ETS转录因子是一类控制细胞增殖、分化和致癌作用的信号依赖性转录调节因子家族。既往研究显示,在约一半的前列腺肿瘤患者中发现了ETS因子ERG与雄激素调节的丝氨酸蛋白酶TMPRSS2的基因融合,其是癌症中最常见的基因重组之一。
TMPRSS2-ERG融合为雄激素诱导的ERG过表达和前列腺上皮细胞转录组的重编程提供了潜在的机制。然而,ERG异常表达影响肿瘤发生发展的相关机制尚不清楚。而了解潜在的发病机制可为该疾病提供新的预后和治疗工具。
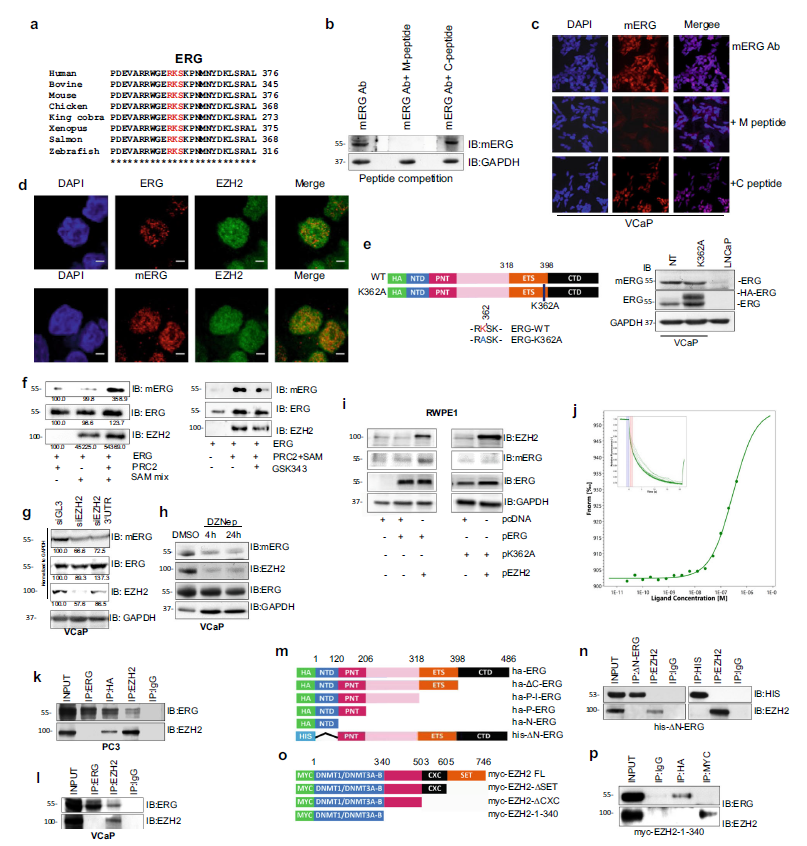
该研究发现了促进ERG致癌活性的重要机制。研究人员发现,ERG的自抑制域内的一个特定赖氨酸残基(K362)能够被EZH2甲基化。机制研究显示,K362甲基化能够改变域内相互作用,有利于DNA的结合并增强ERG的转录活性。
EZH2甲基化ERG K362
在ERG融合阳性前列腺癌的转基因小鼠模型中,ERG K362甲基化与PTEN的缺失和疾病发展为侵袭性腺癌相关。在ERG阳性的VCaP细胞和ERG/PTEN小鼠中,PTEN的缺失能够诱导AKT的激活和EZH2 第21位丝氨酸残基的磷酸化,并有利于ERG的甲基化。
K362甲基化影响蛋白质的构象
进一步的研究发现,ERG能够与EZH2相互作用并共同占据基因组中的几个位点,以形成反式激活复合物。同样的,ERG/EZH2共调节的靶基因在ERG获得和PTEN缺失的肿瘤和去势抵抗性前列腺癌中能够优先的消除该调节作用。
总而言之,该研究结果确定ERG甲基化为一种翻译后修饰,其可维持ERG阳性前列腺癌的发生发展。
原始出处:
Zoma, M., Curti, L., Shinde, D. et al. EZH2-induced lysine K362 methylation enhances TMPRSS2-ERG oncogenic activity in prostate cancer. Nat Commun 12, 4147 (06 July 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#COMMUN#
23
#Nat#
37
#Ezh2#
40
#PRS#
32
#致癌#
33
前列腺癌相关研究,学习了,谢谢梅斯
0