Thorac Cancer:ALK阳性晚期NSCLC患者克唑替尼进展后不同治疗模式的疗效
2022-06-15 yd2015 网络
克唑替尼进展后应用下一代ALK-TKIs显著延长生存期,而序贯使用劳拉替尼似乎更有利。同样,劳拉替尼也延长了第一代和第二代ALK-TKIs失败患者的生存期。
近期,Thoracic Cancer杂志上发表了一项来自我国的回顾性研究成果,主要是评估ALK阳性晚期NSCLC患者克唑替尼进展后不同治疗模式的疗效。

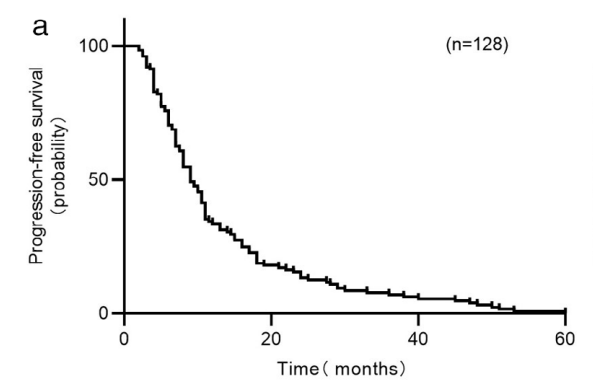
128例患者纳入研究。其中65岁以上12例(9.4%),女性67例(52.3%),33例(25.8%)有吸烟史,50例(39.1%)有骨转移,79例(61.7%)患者接受克唑替尼前接受了至少一个周期化疗。128例患者按照RECIST 1.1评价标准进行评估后,克唑替尼的ORR为68.0%,DCR为93.0%。到最后一次随访时,克唑替尼的中位PFS (mPFS)为9.0个月(95%置信区间[CI],7.7-10.3个月)。中位OS (mOS)为43.0个月(95% CI, 36.9-49.1个月)。

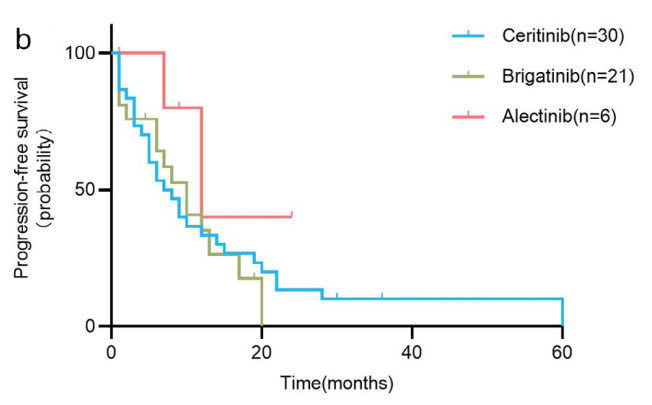
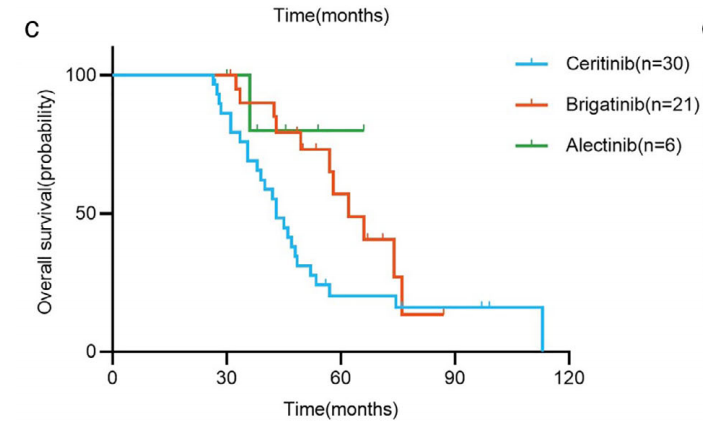
57例患者在克唑替尼耐药后先后接受第二代ALK-TKIs治疗。其中,30例塞瑞替尼患者的mPFS为7.0个月(95% CI, 3.4-10.6个月),mOS为43.0个月(95% CI, 37.7-48.3个月)。21例布加替尼患者的mPFS和mOS分别为10.0个月(95% CI, 6.1-13.9个月)和62.0个月(95% CI, 49.1-74.9个月)。6例阿来替尼患者的mPFS为12.0个月(95% CI, 4.7-19.3个月),mOS未达到(只有1例患者死亡)。组间比较发现序贯布加替尼组的OS明显长于塞瑞替尼组(p = 0.034),其他组间无统计学差异。
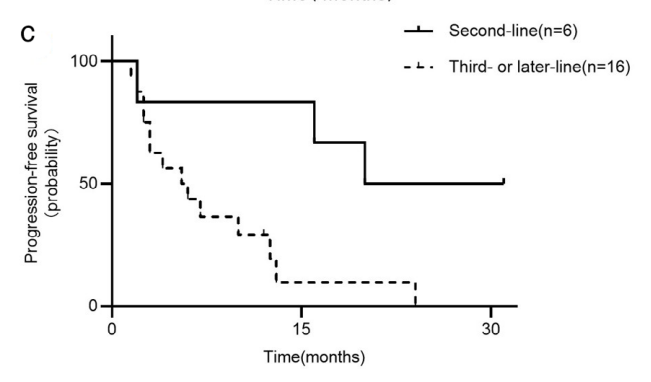
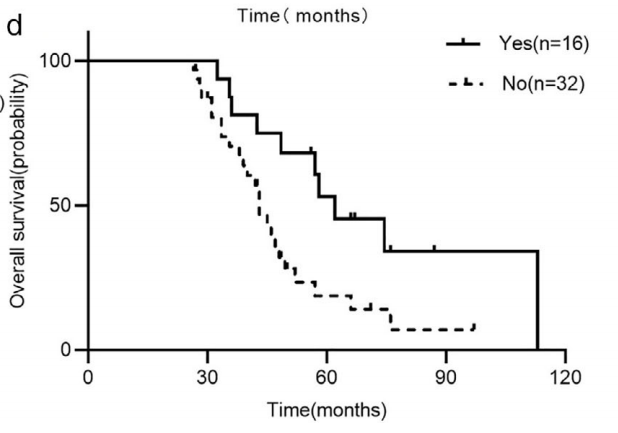
48例患者在第一代和第二代ALK-TKIs治疗后发生疾病进展,其中16例序贯使用劳拉替尼治疗。亚组分析显示,第一代和第二代耐药后,有或没有劳拉替尼治疗患者的OS差异有统计学意义(62.0个月vs. 43.0个月,p = 0.014)。亚组分析显示,不同线数的劳拉替尼治疗对PFS有显著影响(二线:20.0个月vs三线及以后:5.5个月,p = 0.011)。
综上,克唑替尼进展后应用下一代ALK-TKIs显著延长生存期,而序贯使用劳拉替尼似乎更有利。同样,劳拉替尼也延长了第一代和第二代ALK-TKIs失败患者的生存期。
原始出处:
Ma X, Yang S, Zhang K,Xu J, Lv P, Gao H, et al. Efficacy of different sequential patterns after crizotinib progression inadvanced anaplastic lymphoma kinase-positive non–small cell lung cancer. Thorac Cancer. 2022. https://doi.org/10.1111/1759-7714.14455
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#THORAC#
32
#SCLC患者#
37
#ALK阳性#
39
#NSCLC患者#
0
#晚期NSCLC#
34
#治疗模式#
33