AHA 2019|LBS.01 首发四个临床研究:DAPA-HF、ORION-10、COLCOT、 BETonMACE
2019-11-17 MedFocus POCKET AHA2019
2019年11月16日,美国费城,AHA 2019首发四大临床研究: ➤ DAPA-HF试验 ➤ ORION-10 III期试验 ➤ COLCOT试验 ➤ BETonMACE试验
2019年11月16日,美国费城,AHA 2019首发四大临床研究:
DAPA-HF试验
ORION-10 III期试验
COLCOT试验
BETonMACE试验
DAPA-HF
AHA 2019|LBS.01
Background:
Sodium-glucose cotransporter 2 (SGLT2) inhibitors reduce the risk of incident hospitalization for heart failure (HF) in individuals with type 2 diabetes (T2D). Their effects in patients with established HF, including patients without diabetes, are unknown.
Methods:
The key inclusion criteria were: 1) New York Heart Association functional class II-IV, 2) LVEF of 40% or less, 3) plasma NT-proBNP of at least 600 pg/ml (400 pg/ml if hospitalized for HF in prior 12 months or at least 900 pg/ml if atrial fibrillation) and 4) standard drug and device therapy for HF. Key exclusion criteria included type 1 diabetes, symptoms of hypotension or systolic blood pressure below 95 mmHg and estimated glomerular filtration rate (eGFR) below 30 ml/min/1.73m2. The double-blind study treatments were dapagliflozin (10 mg once daily) or matching placebo. We hypothesized that dapagliflozin would be superior to placebo for the primary composite outcome of a first episode of worsening HF (hospitalization for HF or an urgent HF visit requiring intravenous therapy) or death from cardiovascular causes. The secondary outcomes are: 1) the composite of HF hospitalization or cardiovascular death, 2) total number of recurrent HF hospitalizations (including repeat admissions) and cardiovascular deaths, 3) change from baseline to 8-months in the total symptom score of the Kansas City Cardiomyopathy Questionnaire (KCCQ), 4) the incidence of a composite worsening renal function outcome and 5) death from any cause. For the primary endpoint, we assumed a hazard ratio of 0.80 for dapagliflozin compared with placebo.
主要纳入标准:1)纽约心脏协会评价心功能II-IV级,2)左心室射血分数低于40%,3)血浆NT-proBNP大于 600 pg/ml(若过去12个月内因心力衰竭住院,则为400 pg/ml,若有房颤,则为900 pg/ml),4)标准的HF药物和仪器治疗。主要排除标准包括1型糖尿病、低血压症状或收缩压低于95 mmHg以及肾小球滤过率(eGFR)低于30ml/min/1.73m2。治疗方法为达格列净(10 mg,每日一次)或与之匹配的安慰剂。主要假设是,对于首次心衰恶化(因心衰住院或需要静脉治疗的紧急心衰就诊)或心血管原因死亡的主要复合结局,达格列净优于安慰剂。次要终点是:1)心衰住院或心血管死亡的复合终点,2)心衰复发住院(包括重复入院)和心血管死亡的总数,3)堪萨斯城心肌病问卷(KCCQ)评分从基线到8个月的变化,4)合并肾功能恶化的发生率,和5)全因死亡。假设达格列净与安慰剂对于主要终点的危险比为0.80。
Results:
From February 15, 2017, through August 17, 2018, 4744 patients were randomized at 410 centers in 20 countries. The mean age of patients was 66 years and 23% were women. 68% of patients were in NYHA class II, mean LVEF was 31% and the median NT-proBNP 1437pg/ml. 56% of patients had an ischemic etiology and 42% had a history of T2D (45% with T2D when previously undiagnosed T2D included). Mean eGFR was 66 ml/min/1.73m2 and 41% had an eGFR below 60. 94% of patients were treated with a renin-angiotensin system blocker, 96% with a beta-blocker and 71% with an MRA. The trial has completed follow-up, with accrual of the target number of primary endpoints (n=844). The primary results of the DAPA-HF trial will be presented.
从2017年2月15日到2018年8月17日,共纳入来自20个国家410个中心的4744名患者。患者平均年龄66岁,23%为女性。68%为NYHA II级,平均LVEF为31%,NT-proBNP中值为1437 pg/ml。56%的患者有缺血性病因,42%有2型糖尿病病史(包括以前未诊断的2型糖尿病)。平均eGFR为66 ml/min/1.73m2,41%的eGFR低于60。94%的患者使用肾素-血管紧张素系统阻滞剂,96%使用β阻滞剂,71%进行了磁共振血管成像。目前该试验已完成随访,主要终点数目(n=844)。将介绍DAPA-HF试验的主要结果。
Conclusions:
When added to standard therapy, dapagliflozin reduced the risk of worsening heart failure events and cardiovascular death, and improved symptoms, in patients with HFrEF, both with and without T2D. The relative and absolute risk reductions in death and hospitalization were substantial, clinically important, and consistent in patients with and without T2D. Dapagliflozin was well tolerated and the rate of treatment discontinuation was low in patients with and without T2D. Dapagliflozin offers a new approach to the treatment of HFrEF in patients with and without T2D.
在标准治疗的基础上,达格列净降低了HFrEF患者(无论是否伴有T2D)心衰恶化事件和心血管死亡的风险,并改善了症状。死亡和住院的相对风险和绝对风险有实质性的降低,在有和无T2D的患者中一致,具有重要的临床意义。达格列净具有良好的耐受性,停药率低。达格列净为有或无T2D的HFrEF患者的治疗提供了新的途径。
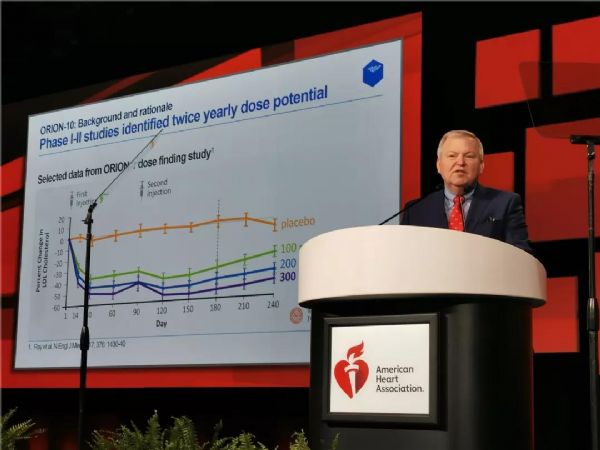
ORION-10
AHA 2019|LBS.01
Background:
Patients with established atherosclerotic cardiovascular disease (ASCVD) are at high risk for cardiovascular events. Low-density lipoprotein cholesterol (LDL-C) is a causal factor for ASCVD and reductions in LDL-C reduce subsequent clinical events. Statins are widely used and require daily dosing. Some patients require additional therapy with daily ezetimibe or twice-monthly injections of a PCSK9-inhibiting monoclonal antibody. There is a need for options with less frequent dosing requirements to improve adherence and compliance. The ORION-1 Phase 2 dose-finding trial suggested that inclisiran, a small interfering RNA (siRNA) targeting hepatic PCSK9 synthesis, has the potential to produce LDL-C reductions of >50% safely, with an infrequent dosing regimen (once every six months). ORION-10 is a Phase 3 trial to assess the efficacy and safety of inclisiran in patients with ASCVD and elevated LDL-C.
动脉粥样硬化性心血管疾病(ASCVD)患者是心血管事件的高危人群。低密度脂蛋白胆固醇(LDL-C)是ASCVD的发病因素,降低LDL-C可减少临床事件的发生。他汀类药物应用广泛,需要每日给药。有些患者需要每日服用依折麦布或每月注射两次pcsk9抑制单克隆抗体进行额外治疗。故有必要减少用药频率来提高依从性。ORION-1二期剂量试验表明,inclisiran,一种靶向肝细胞PCSK9合成的小干扰RNA(siRNA),不频繁给药(每六个月一次)可安全降低50%的LDL-C。ORION-10是一项评估inclisran治疗ASCVD和LDL-C升高患者的疗效和安全性的3期试验。
Methods:
ORION-10 is a Phase 3, placebo-controlled, double-blind, randomized study in 1561 subjects ≥18 years of age with stable ASCVD and elevated LDL-C (≥70 mg/dL) despite maximum tolerated oral statin therapies conducted in the U.S. across 145 sites between December 2017 and September 2019. Subjects were randomized 1:1 to inclisiran sodium 300 mg or placebo, administered at Day 1, Day 90, Day 270 and Day 450. After randomization and the first administration of inclisiran or placebo, patients attended 8 study visits over 18 months for biochemical measurements and to assess safety and tolerability of inclisiran. The co-primary endpoints were the percent change from baseline in LDL-C at Day 510 and the time-adjusted average percentage change from baseline in LDL-C between Day 90 up to Day 540. Key secondary endpoints included the mean absolute change in LDL-C at Day 510, the average absolute reduction in LDL-C between Day 90 up to Day 540, and changes in other lipids and lipoproteins. The proportion of subjects who attain guideline based LDL-C goals was also a pre-specified outcome.
ORION-10是一项3期,安慰剂对照,双盲,随机研究,纳入1561例18岁以上的稳定型ASCVD和LDL-C升高(≥70 mg/dL)患者,尽管2017年12月~2019年9月在美国的145个地区进行了口服耐受性最高的他汀类药物治疗。受试者被1:1随机分组,分别在第1天、第90天、第270天和第450天服用inclisiran 300 mg或安慰剂。在随机化和首次使用inclisiran或安慰剂之后,患者在18个月内参加了8次随访,进行生化测量,并评估inclisran的安全性和耐受性。主要终点是第510天和基线的LDL-C变化百分比,以及从第90天到第540天LDL-C与基线的时间调整平均变化百分比。次要终点包括第510天LDL-C的平均绝对变化、LDL-C在第90天至第540天之间的平均绝对降低以及其他脂质和脂蛋白的变化。达到基于指南的LDL-C目标的受试者比例也是一个预先指定的终点。
Results:
A total of 1561 subjects underwent randomization. Median age was 66 years and the majority were male. Coronary heart disease was present in >90%; between 10 and 20% had prior cerebrovascular disease or peripheral arterial disease. Diabetes was present in approximately 45%. Mean baseline LDL-C was 110 mg/dL, >90% received statins, >80% received high-intensity statins, and ~10% were on ezetimibe.
共有1561名受试者接受了随机分组。中位年龄为66岁,大多数为男性。冠心病的发生率90%,10%至20%有脑血管疾病或外周动脉疾病。糖尿病患者约占45%。平均基线LDL-C为110mg/dL,90%以上使用他汀类药物,80%以上使用高强度他汀类药物,约10%使用依折麦布。
Conclusions:
The safety and efficacy will be presented of 18 months of treatment with inclisiran sodium 300 mg given at Day 1, Day 90 and every 6 months thereafter, compared to placebo, among patients with ASCVD and elevated LDL-C.
在ASCVD和LDL-C升高的患者中,在第1天、第90天和此后每6个月给予含inclisiran钠300 mg治疗18个月的安全性和有效性与安慰剂组相似。
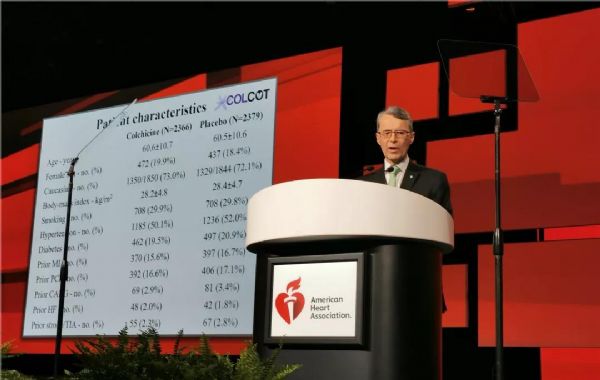
COLCOT
AHA 2019|LBS.01
Introduction:
Multiple lines of evidence have highlighted the important role of inflammation in the pathogenesis of atherosclerosis and its complications. Colchicine is an orally administered, potent anti-inflammatory drug clinically indicated for the treatment of gout and pericarditis.
多种证据表明炎症在动脉粥样硬化及其并发症的发病机制中起着重要作用。秋水仙碱是一种有效的口服抗炎药,临床上用于治疗痛风和心包炎。
Hypothesis:
We hypothesized that colchicine will reduce cardiovascular (CV) events in patients with a recent myocardial infarction (MI).
假设秋水仙碱可以减少心肌梗死患者的心血管事件。
Methods:
The primary objective of COLCOT is to determine if long-term treatment with colchicine 0.5 mg/day will reduce major CV events in patients with a recent MI. The secondary objective is to determine the safety and tolerability of long-term treatment with low-dose colchicine. COLCOT is a randomized, double-blind, placebo-controlled, multi-national clinical trial. A total of 167 clinical sites participated in the trial. Patients were randomly assigned to receive either colchicine (0.5 mg/day) or placebo (1:1 ratio) and followed until at least 301 primary CV events occurred. To enter the trial, adult men and women had to have suffered a MI within the last 30 days and have completed any planned percutaneous revascularization procedures. Follow-up visits occurred at 1 and 3 months following randomization and every ≈3 months thereafter. Patients also received standard medical care including intensive use of statins. The primary study endpoint is the time from randomization to the first event of CV mortality, resuscitated cardiac arrest, non-fatal MI, non-fatal stroke, or urgent hospitalization for angina requiring coronary revascularization. All suspected CV endpoints were adjudicated by an independent and blinded clinical endpoint committee. COLCOT is an event-driven trial with main analyses conducted on an intention-to-treat basis. The sample size calculation was based on the primary endpoint and a hazard ratio of 0.724. Using a two-sided test at the 0.05 significance level, the trial had 80% power if it continued until 301 positively adjudicated primary events occurred in the combined treatment groups. The total number of patients to randomize, 4500, was chosen so that the expected number of adjudicated events after 24 months of follow-up is 301. It assumed an event rate of 7% in the placebo group at 24 months, an 18-month recruitment period, a 24-month minimum follow-up and a 1% yearly lost to follow-up and withdrawal of consent rate.
COLCOT研究的主要目的是确定长期使用0.5毫克/天的秋水仙碱治疗是否能减少心肌梗死患者的主要心血管事件。次要目的是确定长期的小剂量秋水仙碱治疗的安全性和耐受性。COLCOT是一项随机、双盲、安慰剂对照、多国参与的临床试验。共有167个临床中心参与了试验。患者被随机分配接受秋水仙碱(0.5毫克/天)或安慰剂(1:1比率)治疗,且至少需随访301例主要心血管事件。为了进入试验,成年男女必须在过去30天内经历心肌梗死,并完成任意计划的经皮血运重建手术。随机分组后第1个月和第3个月进行随访,此后每≈3个月进行一次随访。患者还接受了标准的医疗护理,包括强化使用他汀类药物。主要研究终点是从随机化后发生的心血管死亡、复苏性心脏骤停、非致命性心肌梗死、非致命性卒中或因心绞痛需要冠状动脉血运重建而紧急住院的时间。所有可疑的心血管终点都由一个独立的临床终点委员会判定。COLCOT是事件驱动型试验,主要分析是在意向治疗的基础上进行的。样本量计算基于主要终点和0.724的危险比。采用双侧0.05显着性水平,如果试验持续到联合治疗组发生301例阳性判定的原发性事件,则试验有80%的效能。随机选择4500名患者,以便在24个月的随访后,预期的判定事件数为301。假设安慰剂组在24个月发生率为7%、同时18个月的招募期、24个月的最低随访期和每年1%的失访率和退出率。
Results:
A total of 4745 patients were enrolled in COLCOT.
共有4745名患者参加了COLCOT研究。
Limitations:
The duration of follow-up was relatively short at approximately 23 months. The risks and benefits of longer-term treatment with colchicine were not evaluated. Although the inclusion of 4745 patients was sufficient to demonstrate a significant benefit on the primary composite efficacy endpoint, a larger trial could have allowed a better assessment of individual endpoints and subgroups and the risks associated with colchicine.
随访时间较短,约23个月。长期使用秋水仙碱治疗的风险和益处没有评估。尽管纳入4745名患者足以证明在主要复合疗效终点有显着益处,但更大规模的试验可以更好地评估个别终点和亚组以及秋水仙碱相关的风险。
Conclusion:
Colchicine 0.5 mg/day significantly reduces the risk of first and total ischemic cardiovascular events by 23% and 34% respectively compared to placebo in patients with a recent myocardial infarction.Rates of adverse effects were low, including a small increase in pneumonias (0.9 vs. 0.4%) but no significant increase in diarrhea with colchicine, on background therapy with aspirin, a 2nd antiplatelet agent and a statin in 99, 98 and 99% of patients.The COLCOT results apply to patients who have recently suffered a myocardial infarction. Further research is needed to assess the benefits of colchicine in other high-risk patients.
与安慰剂组相比,0.5mg秋水仙碱治疗组可显着降低近期心肌梗死患者首次和总缺血性心血管事件的风险,分别降低23%和34%。99%、98%和99%的患者分别有阿司匹林、第二抗血小板药和他汀类药物的用药史,不良反应发生率较低,包括肺炎轻微增加(0.9%对0.4%),但秋水仙碱腹泻无明显增加。COLCOT结果适用于最近发生过心肌梗死的患者。还需要进一步的研究来评估秋水仙碱对其他高危患者的收益。
BETonMACE
AHA 2019|LBS.01
Background:
Bromodomain and extra-terminal (BET) proteins are epigenetic transcription modulators of inflammation, thrombogenesis, and lipoprotein metabolism that contribute to atherothrombosis. BET inhibitors are small molecule epigenetic regulators of chromatin structure and gene expression with therapeutic potential in atherosclerosis. Apabetalone is the first in class BET inhibitor that selectively targets bromodomain 2 (BD2), resulting in favourable effects on transcription of a variety of atherothrombotic mediators. A pooled analysis of phase 2 trials showed that apabetalone reduced the incidence of death or non-fatal cardiovascular (CV) outcomes compared with placebo, with more prominent benefits in patients with conditions associated with BET system activation such as type 2 diabetes mellitus (T2DM), high C-reactive protein or low HDL-cholesterol. The BETonMACE trial tested the hypothesis that addition of treatment with apabetalone to standard of care therapies improves CV outcomes in patients with T2DM and low HDL-C after an acute coronary syndrome (ACS).
Bromodomain和extra-terminal(BET)蛋白是炎症、血栓形成和脂蛋白代谢的表观转录调节剂,可导致动脉粥样硬化血栓形成。BET抑制剂是具有治疗动脉粥样硬化潜力的染色质结构和基因表达的小分子表观遗传调控因子。BET抑制剂Apabetalone选择性靶向于bromodomain 2(BD2),对多种动脉粥样硬化血栓介质的转录产生影响。2期试验分析显示,与安慰剂相比,Apabetalone治疗可降低BET系统激活相关疾病如2型糖尿病(T2DM)、高c反应蛋白或低hdl患者死亡或非致命性心血管疾病(CV)的发生率。BETonMACE试验证实了标准护理加上apabetlone治疗可改善急性冠脉综合征(ACS)后T2DM和低HDL-C患者的CV结局。
Methods:
BETonMACE (NCT02586155) is an international, multi-center, randomized, double-blind, placebo-controlled trial in patients with recent ACS, T2DM and low HDL-C conducted at 195 sites in 13 countries. Patients with ACS in the preceding 7-90 days, T2DM, and HDL-C ≤40 mg/dl for men, ≤45 mg/dl for women, were assigned in double-blind fashion to receive apabetalone 100 mg orally twice daily or matching placebo (1:1) on top of guideline recommended standard of care including intensive or maximum-tolerated treatment with atorvastatin or rosuvastatin. The primary outcome was time to the first occurrence of CV death, non-fatal myocardial infarction (MI), or stroke. The study continued until 250 primary endpoints had accrued. Apabetalone and placebo groups were compared using a two-sided stratified log-rank test; assuming a 2-sided type 1 error rate of 5% and cumulative incidence of the primary endpoint of 10.5% in the placebo arm at 18 months, a sample size of 2400 patients followed for a median of 18 months provides 80% power to detect a 30% relative risk reduction with apabetalone.
BETonMACE(NCT02586155)是一项国际性、多中心、随机、双盲、安慰剂对照试验,纳入了13个国家的195个地区的近期ACS、T2DM和低HDL-C患者。在试验前7-90天出现ACS, 有2型糖尿病,男性HDL-C≤40 mg/dl,女性≤45 mg/dl的受试者中,以双盲的方式分组,在接受阿托伐他汀或瑞舒伐他汀强化或最大耐受治疗的基础上,分别每日口服两次100 mg的apabetalone,或1:1匹配的安慰剂。试验的主要终点是心血管死亡、非致命性心肌梗死(MI)或脑卒中首次出现的时间。研究一直持续到250个主要终点发生。采用双侧分层对数秩检验,比较apabetone组和安慰剂组的差异;假设18个月时安慰剂组的双侧1型错误率为5%,主要终点的累积发生率为10.5%,样本量为2400,平均随访18个月,用 80%的功率来检测使用apabetlone可降低30%的相对风险。
Results:
Enrollment began in November 2015 and ended in July 2018 with 2425 participants randomized. MI was the index ACS event in 74% (STEMI 53%, NSTEMI 47%) with unstable angina constituting 26%. Characteristics of participants included median age 62 years, 25% female sex, majority white race (87%), and coronary revascularization for the index ACS (80%). Use of high intensity statin treatment was 91% at study entry with median LDL-C 65 mg/dl, HDL-C 33 mg/dl, and HbA1c 7.3%. Median follow up was 26 months. Conclusion: The BETonMACE trial will be the first study to report whether epigenetic modulation with a selective BET protein inhibitor is a safe and effective approach to reduce cardiovascular risk.
从2015年11月到2018年7月,共纳入2425名参与者。在74%(STEMI 53%,NSTEMI 47%)的不稳定型心绞痛患者中,MI是ACS的指标性事件,占26%。参与者的中位年龄为62岁,25%为女性,87%为白人,80%进行了冠状动脉血运重建。基线时,高强度他汀类药物的使用率为91%,LDL-C、HDL-Ch和HbA1c的中位数分别为 65 mg/dl , 33 mg/dl和7.3%。中位随访时间为26个月。结论:BETonMACE试验将是首次报道表观遗传调控与选择性BET蛋白抑制剂是否可以安全有效降低心血管风险的研究。
Summary:
Apabetalone did not have a significant effect on incidence of the primary endpoint (CV death, non-fatal MI or stroke).Observed event rate in placebo group (9.7%) was somewhat lower than anticipated (10.5%) at 18 months.Study was powered on a 30% reduction in risk of primary endpoint, and was underpowered to detect a smaller difference in events.Apabetalone was generally well tolerated with an overall incidence of adverse events similar to that in the placebo group. However, discontinuation of treatment due to elevated liver function tests was more frequent with apabetalone.
Apabetalone对主要终点(CV死亡、非致死性心肌梗死或脑卒中)的发生率没有显着影响;18个月时,安慰剂组的事件发生率为(9.7%)略低于预期(10.5%);研究的主要终点风险降低了30%,但不足以检测事件间的较小差异。apabetlone组总体耐受性良好,不良事件发生率与安慰剂组相似。然而,由于肝功能指标升高而中止试验的情况在该组更为常见。
Conclusion:
First cardiovascular outcomes trial assessing the potential of epigenetic modification with BET protein inhibition shows promise.Favorable trends were observed for the primary endpoint and key components except stroke with a nominal difference in heart failure hospitalization.Further studies of this approach are warranted.
这是首次评估BET蛋白抑制表观遗传修饰潜力的心血管结局试验;除卒中外,两组间主要终点及其关键组成部分在心衰住院治疗方面有显着差异,该实验值得进一步研究。
POCKET AHA2019
Immediately
由中国心血管健康联盟和心关注共同发起的POCKET AHA2019项目将依托医望医学提供的人工智能学术跟踪系统,为全国广大心血管医师带来及时全面的报道。
项目得到了医师报、365医学网、国际循环、华迈医学、MedFocus等媒体的大力支持。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#COLCOT#
0
#ACE#
44
#MAC#
30
#BET#
29
#BETonMACE#
38
#AHA#
25
#APA#
33
#MACE#
29